Considering LASIK eye surgery is a significant decision. You’ve likely heard compelling stories about individuals achieving freedom from glasses and contact lenses. However, with any medical procedure, it’s wise to understand every aspect, especially the LASIK Eye Surgery risks. Clear vision is a common goal, but peace of mind is equally important; learning about potential risks empowers you to make an informed choice for your eye health.
A great number of individuals report positive outcomes with laser eye surgery, which boasts a high success rate. Yet, no surgical intervention is completely without risk. Having a frank discussion with your eye doctor about potential complications is crucial for you to fully weigh the advantages against any drawbacks of this laser surgery.

Table of Contents
Understanding LASIK: A Quick Refresher
Before exploring potential problems, it’s helpful to review what LASIK eye surgery entails. LASIK, an acronym for Laser-Assisted In Situ Keratomileusis, is a widely performed type of refractive surgery. This laser vision correction technique aims to rectify vision problems such as nearsightedness (myopia), farsightedness (hyperopia), and astigmatism, ideally reducing or negating the need for glasses or contact lenses.
The laser eye surgery involves a specialized laser creating a precise, thin flap in the cornea, the transparent front surface of your eye. Another laser, an excimer laser, then carefully reshapes the corneal tissue beneath this flap. After the cornea is appropriately contoured, the flap is repositioned and heals naturally, allowing light to focus correctly on the retina for improved laser vision.
This advanced form of eye care, specifically situ keratomileusis, has transformed vision correction for many. The goal is to provide a long-term solution for refractive error, contributing to healthy eyes. It’s an effective procedure for many, but understanding the process is the first step before considering the LASIK risks.
Common (And Usually Temporary) Side Effects After LASIK
Following LASIK surgery, it is common for patients to experience certain side effects as their eyes heal. Most of these are temporary, generally improving within several weeks or months. Understanding what to anticipate can make the surgery recovery period less anxious for patients to talk about these issues openly.

Dry Eyes
Dry eye syndrome is one of the most common side effects after LASIK surgery. Patients might notice their eyes feeling gritty, scratchy, or generally uncomfortable, sometimes accompanied by a burning sensation or redness. These symptoms of dry eyes can significantly impact comfort, particularly in dry environments or during prolonged screen use.
The condition of dry eye occurs because the laser eye surgery can temporarily diminish tear production and alter corneal nerve sensitivity, which are crucial for stimulating tears. Your eye doctor will likely prescribe lubricating eye drops, often preservative-free, to be used frequently post-procedure. In many cases, these LASIK symptoms of dry eyes resolve or substantially improve within three to six months, but a small percentage of individuals may experience persistent dry eye requiring ongoing management.
For those with more stubborn dry eye, additional treatments might be considered, such as punctal plugs, which block tear ducts to keep eyes moister, or prescription medications to increase tear production. Maintaining good hydration and using a humidifier can also offer some relief. It’s important for patients experiencing persistent dry eye symptoms to discuss them with their LASIK surgeon, as chronic dryness can affect vision quality and overall eye health if not addressed; these discussions should include dry eye management strategies.
Related Article
Managing Dry Eye Syndrome: Causes and TreatmentsGlare, Halos, and Starbursts
Visual disturbances such as halos around lights, glare from sources like oncoming headlights, or starburst patterns (collectively referred to as glare halos) are frequently reported, particularly during night driving or in low-light conditions. These visual symptoms are common during the initial healing phase of surgery recovery. They arise from the interaction of light with the reshaped cornea and any temporary post-operative swelling, and in some cases can cause what appears to be double vision under specific lighting.
For most individuals undergoing LASIK eye surgery, these night vision problems tend to diminish progressively as the eyes heal over several weeks to months. However, a minority of patients might find that some degree of these visual symptoms persists longer. This can be particularly concerning for individuals like a police officer or others who rely heavily on clear night vision for their occupation.
Pre-operative assessment of your pupil size, especially in dim light (scotopic conditions), is an important step, as larger pupils can sometimes be associated with a higher likelihood of these night vision issues. Openly discussing any pre-existing difficulties with night vision or concerns about these potential risks with your eye doctor is vital before you undergo LASIK. An experienced LASIK surgeon will consider these factors in your evaluation for LASIK surgery.
Light Sensitivity
An increased sensitivity to light, medically termed photophobia, is another possible side effect following LASIK eye surgery. Bright sunlight or even standard indoor lighting might appear more intense or uncomfortable than before the procedure. Using sunglasses, particularly when outdoors, can effectively help manage this sensitivity during the healing period.
This light sensitivity generally subsides significantly within the first few days to weeks as part of the natural surgery recovery process. Your cornea is adjusting to its new shape, and this temporary sensitivity is a common response. If photophobia is severe or prolonged, it is important to consult your eye care professional.
Blurry or Fluctuating Vision
It is quite normal for your vision to be somewhat blurry or to vary during the initial days or even weeks after your LASIK eye procedure. Your eyes are undergoing a healing process, and it takes time for your vision correction to stabilize. You might observe that your vision clarity differs at various times of the day or from one day to the next.
Patience during this phase of surgery recovery is important. Avoid discouragement if your vision isn’t immediately crystal clear. Most individuals discover their vision progressively improves as the healing continues and their healthy eye adjusts to the changes from the laser surgery.
Related Articles
Blurry Vision after LASIKMore Serious LASIK Eye Surgery Risks To Consider
Although many side effects are transient, there are also more significant LASIK eye surgery risks. These potential risks are less common, but awareness is vital. A comprehensive pre-operative screening is designed to identify individuals who might have an increased susceptibility to these LASIK complications or poor outcomes.

| Issue Type | Examples | Typical Onset/Duration | Commonality | Management/Resolution |
|---|---|---|---|---|
| Common Temporary Side Effects | Dry eyes, glare, halos, starbursts, light sensitivity, blurry/fluctuating vision | Days to weeks/months post-surgery | Common to Very Common | Eye drops, time, sunglasses; usually resolve as the eye heals. Include dry eyes management in post-op care. |
| More Serious (Less Common) Risks | Under/over-correction, new/worsened astigmatism, flap complications, infection, corneal ectasia, significant or permanent vision loss/changes, persistent double vision | Can be immediate, gradual, or appear months/years later (e.g., ectasia) | Uncommon to Rare | May require enhancement surgery, medication, specialized contact lenses, or in rare cases, corneal transplant. Some may be permanent; prompt reporting of lasik symptoms is critical. |
Under-correction or Over-correction
Occasionally, the excimer laser may remove an insufficient amount of corneal tissue, leading to under-correction, or an excessive amount, resulting in over-correction. If either occurs, your vision will not be as sharp as anticipated post-LASIK surgery. You might find yourself still needing glasses or contact lenses, although typically with a much weaker prescription than prior to the laser eye surgery.
In certain situations, an enhancement procedure, which is essentially a repeat LASIK surgery, could be offered to refine the visual outcome. The suitability for such a procedure depends on various factors, including the stability of your current vision and sufficient remaining corneal thickness. Your LASIK surgeon will discuss this possibility with you if it is deemed necessary and safe to improve outcomes.
Astigmatism
LASIK eye surgery can, in some instances, induce new astigmatism or exacerbate pre-existing astigmatism. Astigmatism results from an irregularly shaped cornea or lens, leading to blurred or distorted vision at all distances, and in some cases, symptoms like double vision or eye strain. This particular LASIK complication can occur if the corneal tissue ablation is uneven or if the corneal flap does not heal with perfect alignment.
Similar to under-correction or over-correction, the development or worsening of astigmatism may necessitate continued use of corrective lenses like glasses or specialized contact lenses. An enhancement procedure might be an option to correct this induced astigmatism, pending a thorough evaluation by your eye doctor. Addressing these visual symptoms promptly is part of good eye care.
Flap Complications

The corneal flap created during the LASIK eye procedure is integral, but it can, albeit rarely, be a source of LASIK complications. Potential issues include improper adherence of the flap, displacement (especially due to eye rubbing or trauma), or the development of microscopic wrinkles or striae on the flap. These flap-related problems can negatively impact vision quality, sometimes causing blurry or distorted vision, or even double vision if the flap is significantly misaligned or wrinkled.
A rare but notable flap complication is diffuse lamellar keratitis (DLK), colloquially known as “Sands of the Sahara.” DLK involves inflammation occurring beneath the flap, which can lead to hazy vision if not managed swiftly with medicated eye drops, typically corticosteroids. Strict adherence to post-operative care, particularly avoiding any rubbing of the eyes, is crucial to minimize these potential risks and support healing of the small incision area where the flap was created.
Other flap issues, though infrequent, include epithelial ingrowth, where cells from the cornea’s surface grow underneath the flap, potentially affecting vision. While some alternative procedures like PRK or small incision lenticule extraction (SMILE) avoid creating a flap, they have their own set of considerations. Careful patient selection and surgeon skill help reduce the LASIK complication rate associated with flaps.
Infection
All surgical procedures carry some risk of infection, and LASIK surgery is not exempt from this possibility. Although eye infections are uncommon following laser eye surgery (with a low complication rate cited by many medical professionals), they can be serious. If not treated promptly, an infection could potentially threaten vision, leading to poor outcomes.
Signs of a possible eye infection include escalating pain, increased redness, unusual discharge from the eye, and a noticeable decline in vision. You will be prescribed antibiotic eye drops for use after your laser surgery to help prevent such infections. Maintaining rigorous hygiene, such as thoroughly washing your hands before touching your eyes or administering any eye drops, is also a fundamental preventive measure to protect your eye health.
Corneal Ectasia

Corneal ectasia represents a very serious, albeit rare, LASIK complication. This condition involves a progressive weakening, thinning, and bulging of the cornea post-surgery, leading to significant vision impairment. Management often requires specialized hard contact lenses or, in advanced cases, a corneal transplant to restore vision.
Ectasia can manifest months or even years after the initial LASIK eye surgery. A primary purpose of comprehensive pre-operative corneal imaging and mapping (topography and tomography) is to identify individuals at higher risk. This includes those with congenitally thin corneas or subtle, pre-existing signs of keratoconus, a corneal thinning disorder which itself is a contraindication for laser vision correction via LASIK due to the heightened risk of ectasia.
Identifying good candidates through meticulous screening is paramount to avoiding such severe vision problems. If there’s any suspicion of corneal irregularity, alternative vision correction methods that do not involve thinning the cornea, or that may even strengthen it, would be discussed by your eye doctor. Understanding these potential risks is vital before you undergo LASIK.
Related Article
Can You Get LASIK with Thin Corneas? Risks and AlternativesVision Loss or Changes
Although exceedingly rare, there is a possibility of experiencing some degree of vision loss or irreversible visual changes that cannot be rectified with glasses, contact lenses, or subsequent surgical interventions. This could mean that your best-corrected visual acuity (the sharpest vision achievable with corrective lenses) is diminished compared to your pre-LASIK state. While severe, permanent vision loss is an exceptionally uncommon result of laser eye surgery, it remains a documented potential risk that warrants consideration.
This possibility highlights the critical importance of selecting a highly experienced LASIK surgeon and undergoing an exhaustive pre-operative evaluation to confirm you are among the good candidates for the procedure. Having an open dialogue about all potential LASIK Eye Surgery risks and any expected complications with your eye doctor is fundamental to making a well-informed decision regarding this vision correction surgery. This conversation should cover your individual LASIK complication rate likelihood.
Factors That Can Influence LASIK Eye Surgery Risks
Not every individual is an ideal candidate for LASIK. Various factors concerning your eye health, general physical health, and even certain lifestyle choices can affect your suitability for this laser surgery. These elements also influence the potential for LASIK Eye Surgery risks, and a comprehensive evaluation by medical professionals will assess these aspects.
Pre-existing Eye Conditions
Specific eye conditions can elevate LASIK risks or render an individual unsuitable for the laser eye procedure. For instance, if you suffer from severe dry eye syndrome, undergoing LASIK could potentially exacerbate this condition significantly. Disorders like keratoconus, characterized by progressive corneal thinning, are generally considered contraindications for LASIK due to the substantial risk of inducing corneal ectasia, a serious LASIK complication.
Other eye health issues such as uncontrolled glaucoma, active or recurrent eye infections (e.g., ocular herpes simplex), significant corneal dystrophies or diseases, and certain retinal conditions require careful evaluation. If you have cataracts, your eye doctor might suggest addressing the cataract first, as cataract surgery inherently includes vision correction and might make subsequent LASIK unnecessary. All existing eye conditions must be disclosed and discussed.
Overall Health Conditions
Your overall systemic health significantly influences healing and potential risks associated with LASIK eye surgery. Uncontrolled autoimmune diseases, such as lupus or rheumatoid arthritis, can impede the body’s healing mechanisms and heighten the risk of complications. Similarly, poorly managed diabetes can adversely affect ocular healing processes and elevate the likelihood of infection and other adverse events following surgery.
Medications that suppress the immune system, often prescribed for autoimmune conditions or after organ transplants, can also impact the healing trajectory and susceptibility to infection. It is critically important to provide your eye doctor with a comprehensive and accurate medical history. This helps them determine if laser vision correction is a safe option for you and how to improve outcomes.
Pupil Size
Individuals with naturally large pupils, particularly in low-light (scotopic) conditions, may face an increased probability of experiencing night vision problems post-LASIK. These issues can include bothersome glare halos, starbursts around lights, or reduced contrast sensitivity. While advanced laser technology and sophisticated screening methods have helped reduce this risk, pupil diameter remains an important factor your LASIK surgeon will carefully assess during your pre-operative evaluation.
The measurement of pupil size in varying light conditions helps predict the likelihood of these visual symptoms. If you have significantly large pupils, your surgeon might discuss the potential for these night vision disturbances or suggest alternative vision correction options. This careful assessment helps manage expectations regarding potential LASIK symptoms.
Corneal Thickness
The LASIK surgery procedure involves the precise removal of a minute amount of corneal tissue to reshape it for better vision. If your corneas are inherently thin, ablating additional tissue could compromise corneal integrity, thereby weakening it and escalating the risk of severe complications such as corneal ectasia. An accurate measurement of corneal thickness, known as pachymetry, is therefore a critical component of the pre-operative assessment to determine if you are one of the good candidates.
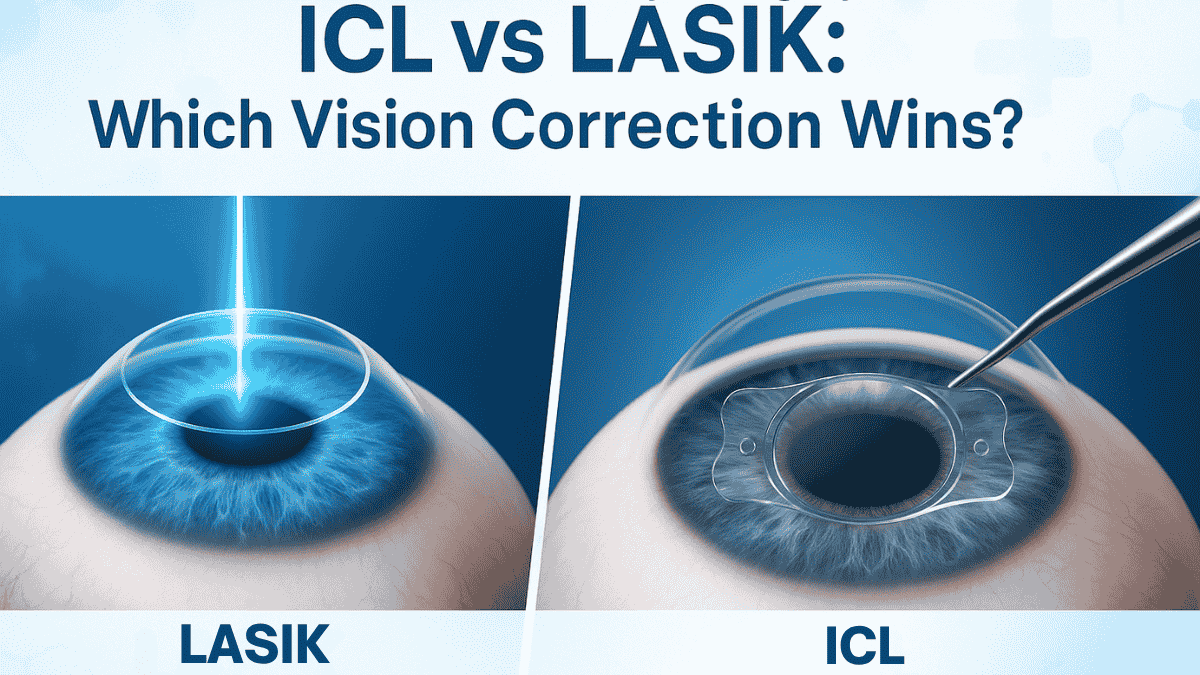
Should your corneas be deemed too thin for LASIK, your eye doctor will discuss alternative refractive surgery options. These might include Photorefractive Keratectomy (PRK), which is a surface ablation procedure, or implantable collamer lenses (ICLs), which are like permanent contact lenses placed inside the eye. These alternatives may offer a safer path to vision correction for individuals with thin corneas, as some, like ICLs, do not involve removing corneal tissue, while PRK removes less or allows for safer treatment of thinner corneas.
Another alternative, small incision lenticule extraction (SMILE), is a newer form of laser eye surgery that involves creating a lenticule (a small, lens-shaped piece of tissue) within the cornea, which is then removed through a small incision. This procedure, known as incision lenticule extraction, may be an option for some patients not suitable for traditional LASIK, as the incision lenticule is smaller. Understanding these options involving small incision lenticule techniques is part of comprehensive eye care.
Age and Stable Vision
Generally, candidates for LASIK eye surgery should be at least 18 years of age, though some surgeons prefer patients to be slightly older, typically in their early twenties, to better confirm vision stability. A critical requirement is that your eyeglass or contact lens prescription has remained stable for at least one year, and preferably two, before you undergo LASIK. If your vision is still actively changing, the corrective effects of the laser vision procedure may not be durable, leading to a need for further correction sooner than anticipated.
Significant hormonal fluctuations, such as those experienced during pregnancy or while breastfeeding, can also induce temporary shifts in vision. Consequently, LASIK is generally not recommended during these periods. It is best to wait until your vision has demonstrated consistent stability for an extended period, which is vital for achieving predictable and lasting results from the laser eye surgery and is something older adults considering the procedure should also confirm with their medical professionals.
Lifestyle Choices
Your lifestyle choices and occupational demands can also influence both your suitability for LASIK and potential long-term outcomes. If you actively participate in high-impact contact sports or have a profession with a significant risk of eye trauma (e.g., a police officer or military personnel), this requires a thorough discussion with your LASIK surgeon. While the corneal flap created during LASIK heals securely for most daily activities, a direct, forceful impact to the eye, especially during the early surgery recovery phase, carries a risk of flap displacement.
Understanding how your routine activities, hobbies, and work environment might affect your LASIK recovery and the long-term integrity of your vision correction is an essential part of the consultation process. Some patients might be advised to consider alternative procedures like PRK, which does not involve creating a flap and may be considered more robust for certain high-risk activities. Making an informed decision includes evaluating these LASIK risks against your lifestyle.
Reducing Your LASIK Eye Surgery Risks: What You Can Do
Although no surgical procedure is entirely free of risk, you can take proactive steps to help minimize the potential for LASIK Eye Surgery risks. Much of this involves being thoroughly informed and an active participant in your eye care. While social media can offer insights into what patients experience, always consult directly with medical professionals for factual information. Advocating for your own healthy eyes is important throughout the process of considering any laser eye surgery.
Choosing a Skilled and Experienced Surgeon
Selecting a skilled and experienced LASIK surgeon is arguably one of the most critical decisions you will make. Seek out a board-certified ophthalmologist who has substantial experience specifically in performing LASIK and other forms of refractive surgery. Do not hesitate to inquire about their credentials, the volume of procedures they have completed, their personal LASIK complication rate, and their approach to managing any potential complications.
A reputable surgeon will welcome your questions, provide transparent answers, and conduct a thorough pre-operative evaluation, not merely a cursory screening. Feeling confident and trusting your chosen experienced LASIK surgeon is paramount, as they will guide you through the entire laser eye surgery process. When you search, search for patient testimonials and reviews from credible sources, but remember that direct consultation is most important.
You might also ask about the specific laser technology they use and how it contributes to making the LASIK safe and an effective procedure with positive outcomes. Discussing what to expect complications wise, even if rare, shows a surgeon’s commitment to informed consent. Good medical professionals will prioritize your understanding and comfort.
Thorough Pre-operative Evaluation
A comprehensive eye examination and detailed pre-operative evaluation are absolutely essential to ascertain if you are among the good candidates for LASIK eye surgery. This assessment should encompass precise measurements of your refractive error, corneal thickness (pachymetry), corneal shape and curvature (topography/tomography), pupil diameter in various lighting, tear film assessment for dry eye, and a thorough check of your overall eye health. This meticulous screening aids in identifying any underlying factors that could elevate your risk of LASIK complications.
This evaluation also serves as a crucial opportunity for an in-depth conversation with your eye doctor about your specific visual aspirations, lifestyle considerations, and any anxieties or questions you may have regarding the LASIK procedure. Setting realistic expectations about the outcomes and potential limitations of laser vision correction is fundamental to achieving satisfaction with the results. Patients talk about the importance of this consultation for their peace of mind.
Following Pre- and Post-Operative Instructions Carefully
Your LASIK surgeon will provide detailed instructions for both the pre-operative and post-operative phases of your LASIK eye experience. These directives will cover important aspects such as when to discontinue wearing contact lenses prior to your evaluation and the surgery itself, the correct method for administering prescribed eye drops, and a list of activities to avoid during the critical healing period. Strict adherence to these guidelines is vital for facilitating a smooth surgery recovery and minimizing potential LASIK risks.
For instance, consistently using your antibiotic and anti-inflammatory eye drops as directed is essential for preventing infection and managing inflammation, which helps improve outcomes. Similarly, conscientiously avoiding rubbing or putting pressure on your eyes is crucial for protecting the corneal flap and allowing it to heal undisturbed. Following all guidance contributes to a safer laser eye surgery journey.
Reporting Symptoms Promptly
Following your laser surgery, it is important to be vigilant about how your eyes feel and the quality of your vision. Should you experience any unusual LASIK symptoms, such as escalating pain, marked redness, any form of discharge, a sudden deterioration in vision, or if anything simply feels amiss, contact your surgeon’s office without delay. Prompt detection and early treatment of potential complications can significantly influence the final outcome and help avoid poor outcomes.
Never assume that a concerning symptom is “normal” or will resolve on its own if it worries you. It is always preferable to have it evaluated by your eye care professional to address any LASIK complication quickly. Your healthy eye and vision depend on this proactive approach.
Long-Term Considerations and LASIK Eye Surgery Risks
Considering LASIK eye surgery also involves looking at the long-term picture. While LASIK strives to offer durable vision correction, your eyes and vision can naturally change over time due to aging or other health factors. It is beneficial to have a realistic understanding of what to anticipate years after your laser vision correction procedure.
Presbyopia
LASIK is an effective procedure for correcting existing distance vision problems such as nearsightedness, farsightedness, and astigmatism. However, it does not prevent presbyopia, the natural age-related decline in near vision that commonly begins to affect individuals, including older adults, in their early to mid-forties. This means that even after successful laser eye surgery for distance, you will likely require reading glasses for tasks like reading small print as you age.
Some individuals opt for a monovision LASIK approach, where one eye (typically the dominant one) is corrected for clear distance vision, and the other eye is intentionally left slightly nearsighted for better near vision. This can reduce or delay the need for reading glasses but is a compromise that involves adaptation and may not be suitable for everyone. A thorough discussion with your eye doctor is essential to see if this strategy aligns with your visual needs and lifestyle, especially considering the potential impact on depth perception or clear vision for specific tasks.
Potential Need for Future Enhancements
Although LASIK results are typically stable for many years, subtle changes in vision can occur over time due to natural aging or other factors. In some instances, an individual who underwent LASIK years prior might notice a slight regression or blurriness in their vision. If this change is visually significant, an enhancement procedure (a repeat LASIK or PRK) could be considered, assuming sufficient corneal thickness remains and the eye is otherwise healthy and a good candidate.
It is not a certainty that an enhancement will be feasible or recommended years down the line; each case is unique. Consistent, regular eye examinations with your eye care provider are important for monitoring your vision and overall eye health long-term. This continued eye care helps in early detection of any changes and discussion of potential options.
Cataract Surgery Later in Life
LASIK eye surgery does not prevent the development of cataracts, a common age-related condition where the eye’s natural lens becomes cloudy, affecting vision. If you develop cataracts later in life and require cataract surgery, your history of having undergone LASIK is crucial information for your cataract surgeon. Prior laser vision correction can make the calculations for selecting the appropriate power of the intraocular lens (IOL) implanted during cataract surgery more challenging.
Retaining your pre-LASIK and immediate post-LASIK medical records, specifically detailing your prescription before LASIK and the changes made, can be immensely helpful for your cataract surgeon. While advancements in IOL calculation formulas and diagnostic technology have significantly improved the accuracy of outcomes for cataract surgery recovery in post-LASIK patients, it remains an important factor. Proper planning ensures the best possible visual outcome after removing the cataract and implanting the new lens.
Medical professionals specializing in cataract surgery are familiar with these considerations. Discussing your LASIK history thoroughly helps them choose the best approach and IOL type for your specific needs, aiming to restore clear vision and potentially address any remaining refractive error from the original laser eye surgery.
Related Article
Laser Eye Surgery Age Limits: What Parents Should KnowConclusion
LASIK eye surgery can be a life-changing procedure for many, offering freedom from glasses and contact lenses. Millions have benefited from clearer vision. But, it’s essential to go into it with your eyes wide open, fully understanding the potential LASIK Eye Surgery risks and side effects. While serious complications are not common, they can happen, and being aware helps you make an informed and confident decision. Discussing all these LASIK Eye Surgery risks thoroughly with a qualified eye surgeon is the most important step you can take towards a successful laser vision correction experience.
Related Article
Is Laser Eye Surgery Worth It? Exploring the Benefits
Common side effects after LASIK include dry eyes, temporary vision fluctuations, glare, halos around lights, and light sensitivity. These effects are typically mild and resolve within a few weeks. However, some patients may experience them for a longer period depending on their individual healing response and adherence to post-op care.

Yes, in rare cases, LASIK can lead to chronic dry eye symptoms. The surgery may temporarily disrupt tear production by affecting corneal nerves. Most patients experience improvement within 6 months, but a small percentage may require ongoing treatment such as artificial tears or punctal plugs.

Although extremely rare, severe vision loss can occur due to complications like infection, flap issues, or corneal ectasia. Most reputable surgeons have less than 0.1% complication rates for vision loss. Choosing an experienced provider and undergoing proper screening greatly reduces this risk.

Halos and glare are common visual disturbances after LASIK, especially at night. They usually diminish within the first few weeks to months post-surgery. For some individuals, these effects may persist longer, especially if they have larger pupils or pre-existing night vision issues. Advances in LASIK technology have significantly reduced the occurrence of these symptoms.

Yes, night vision problems such as reduced contrast sensitivity or glare from lights can occur after LASIK. These effects are typically most noticeable in the early healing phase and tend to improve with time. In rare cases, advanced LASIK technologies like wavefront-guided procedures may be recommended to reduce such complications.

Flap dislocation occurs when the thin corneal flap created during LASIK shifts from its position before it fully heals. It’s a rare complication, usually caused by trauma or rubbing the eyes soon after surgery. Surgeons take great care to position the flap securely, and patients are advised to avoid eye contact for several weeks.

Yes, increased light sensitivity is a frequent temporary effect after LASIK. It often resolves within weeks, but in some individuals it may linger longer. Wearing sunglasses and avoiding direct sunlight can ease the discomfort. Photophobia that persists should be evaluated by a specialist.

While most LASIK outcomes are stable, potential long-term risks include ectasia (corneal bulging), regression (vision worsening over time), or chronic dry eye. These are uncommon, especially with proper screening and modern techniques. Patients with healthy corneal thickness and no underlying issues are at very low long-term risk.

Yes. Despite precise calculations, some patients may not achieve perfect vision initially and require enhancement. Undercorrection is more common in high prescriptions, while overcorrection is rarer. Follow-up assessments help determine if additional laser adjustment is needed.

Yes, LASIK permanently removes corneal tissue to reshape the eye. This reduces total thickness, which can pose risks if the cornea was already thin. Proper pre-op measurements and conservative correction levels help minimize this issue. Patients with keratoconus or very thin corneas may not be good candidates.

Enhancement surgeries, or LASIK touch-ups, are needed in approximately 5–10% of patients, often due to slight regression or undercorrection. These procedures are usually done months or years after the initial surgery and can further improve vision clarity. Surgeons will monitor outcomes during follow-ups to determine if enhancement is appropriate.

Although rare, LASIK can lead to infections or inflammation, especially if aftercare instructions are not followed. Infections like diffuse lamellar keratitis (DLK) require immediate treatment to prevent complications. Using prescribed antibiotic and steroid eye drops as directed significantly lowers the risk.

Some patients report increased anxiety or depression after LASIK, especially if results are not as expected. Visual disturbances or complications may contribute to emotional stress. However, such psychological effects are rare and often improve with time or counseling. Setting realistic expectations before surgery helps reduce disappointment.

LASIK itself does not cause vision to worsen, but natural age-related changes or underlying conditions like presbyopia may affect vision later. In rare cases, complications like corneal ectasia can lead to declining vision. Regular checkups help track long-term outcomes and catch any issues early.

Yes, some patients may experience double vision (diplopia) if the eye heals unevenly or if there’s a flap issue. This is typically temporary and resolves with healing, but persistent double vision should be evaluated. Advanced imaging and follow-up exams can identify causes and treatment options.

Corneal ectasia is a rare but serious complication where the cornea becomes progressively thinner and begins to bulge outward, distorting vision. It can occur when too much corneal tissue is removed or if the patient has undiagnosed keratoconus. Pre-surgical screening and conservative laser settings significantly reduce this risk.

LASIK is typically used to correct astigmatism, but in rare cases, irregular healing or laser calibration issues can induce or worsen astigmatism. This may require a second procedure or the use of corrective lenses. Accurate mapping and experienced surgeons minimize this risk.

Flap complications include incomplete flaps, flap wrinkles (striae), or epithelial ingrowth under the flap. These are uncommon with current technology but can affect visual outcomes if not promptly treated. Following the surgeon’s post-op instructions is crucial for proper healing.

Yes, although LASIK corrects existing vision problems, age-related changes like presbyopia may require reading glasses later. Also, mild regression can occur over time, especially in people with high prescriptions. Regular follow-up and enhancements help maintain visual clarity.

Yes. People with thin corneas, autoimmune conditions, dry eyes, or high prescriptions may face increased risks. Pre-surgical evaluations help determine candidacy and minimize potential complications. It’s important to disclose your full medical history to your eye surgeon.