Dry eye can be a real pain, making your eyes feel gritty and irritated. If you’re dealing with itchy, burning eyes that feel like they’re full of sand, you’re not alone in experiencing these common dry eye symptoms. Millions of people struggle with this prevalent eye condition, often referred to as dry eye syndrome, every day, impacting their quality of life and ability to perform daily tasks. But don’t worry – there are plenty of ways to find relief and get your eyes feeling comfortable again, addressing the discomfort that makes your eyes feel uncomfortable.
This guide explores various aspects of dry eye disease. You’ll learn what contributes to decreased tear production or increased tear evaporation, how to spot the eye symptoms, and most importantly – what you can do to treat it effectively. We’ll examine home remedies, over-the-counter options like artificial tears, and when an eye exam with a specialist is necessary for this ocular surface disease. By the end, you’ll have a comprehensive understanding and strategies to tackle dry eye head-on and improve your eye care routine.
Ready to say goodbye to irritated eyes and understand why your eyes feel this way? Let’s explore the details of dry eye together, a condition sometimes known by its medical term, keratoconjunctivitis sicca.
Table of Contents
What Exactly Is Dry Eye?
Dry eye, or dry eye syndrome, occurs when your eyes do not produce enough tears, or when the tears evaporate too quickly from the eye’s surface. This lack of adequate lubrication leaves the ocular surface vulnerable and without the necessary moisture it needs to function properly. The result is often discomfort, fluctuating blurry vision, and that persistent gritty feeling in your eyes that makes them feel uncomfortable.
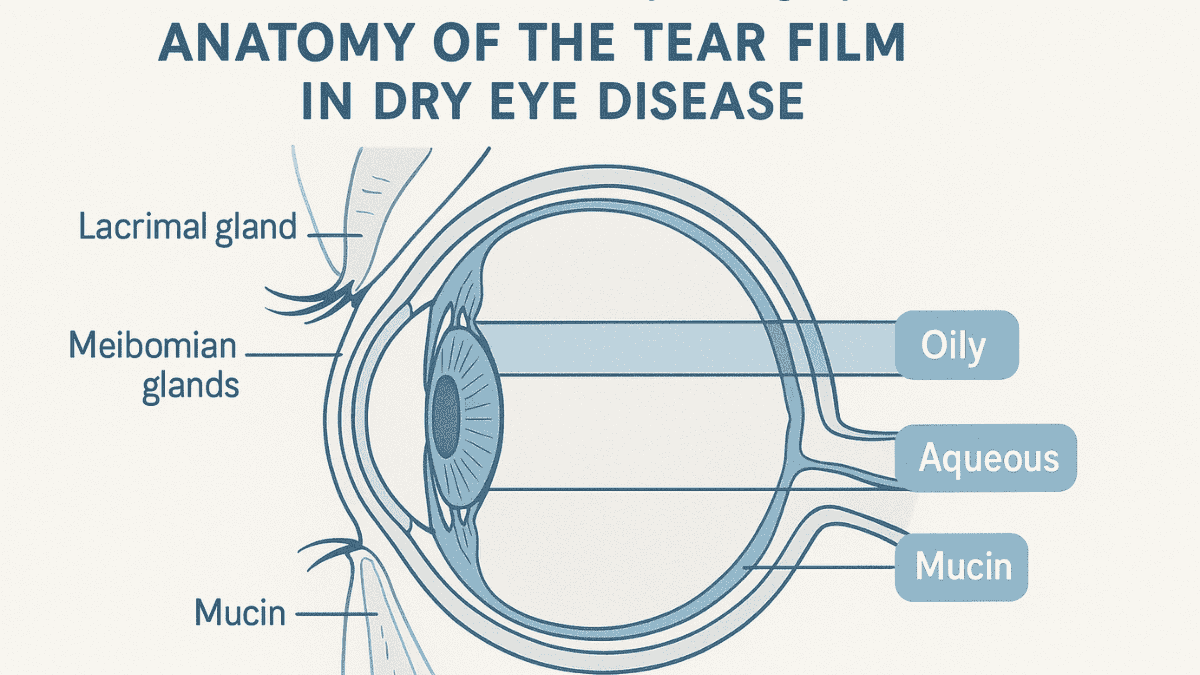
Your tears are more than just water; they are a complex mixture essential for eye health, forming a protective tear film. This tear film, produced by various glands including the lacrimal glands and meibomian glands, consists of three layers: an oily outer layer, a watery middle layer (aqueous fluid), and a mucousy inner layer. When this delicate balance is disrupted, perhaps due to meibomian gland dysfunction or issues with the tear glands, dry eye can develop, impacting the stability of the film produced.
The stability of the tear film is crucial for maintaining a healthy ocular surface and clear vision. Factors leading to decreased tear production or increased tear evaporation can compromise this stability, leading to surface disease. Understanding the components and function of your tears helps in appreciating how various factors can lead to dry eye disease.
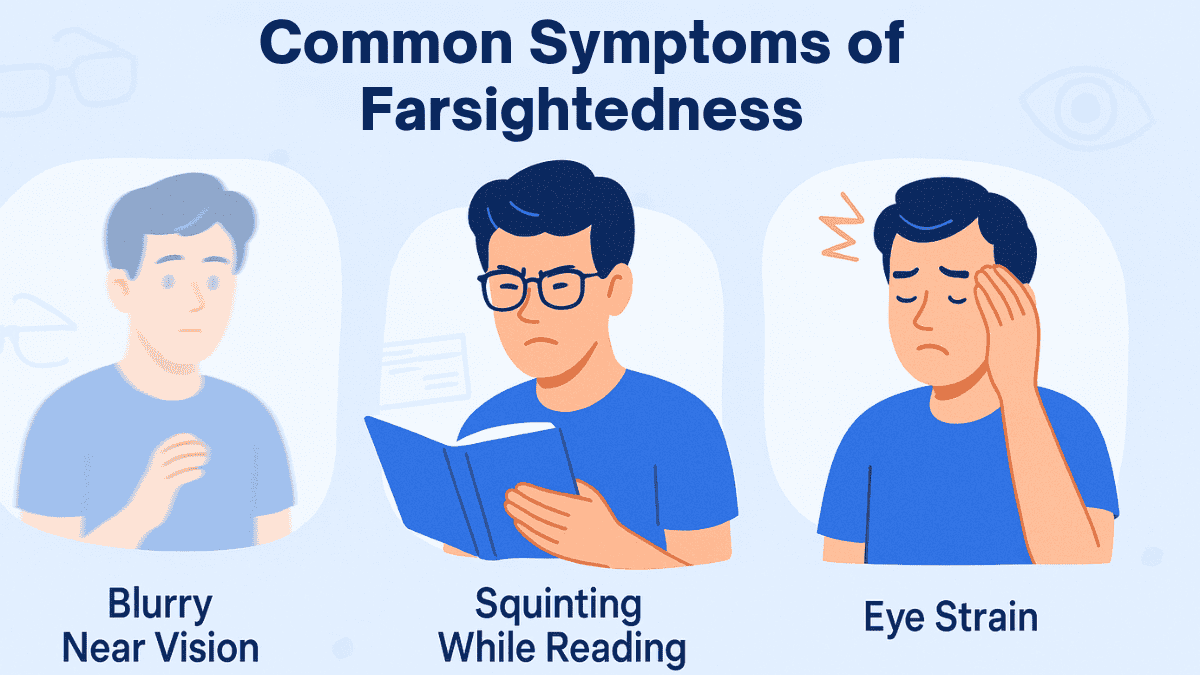
Common Symptoms of Dry Eye
How do you know if you have dry eye syndrome? Recognizing the signs early can lead to quicker relief. Common dry eye symptoms often make your eyes feel uncomfortable and can interfere with daily activities.
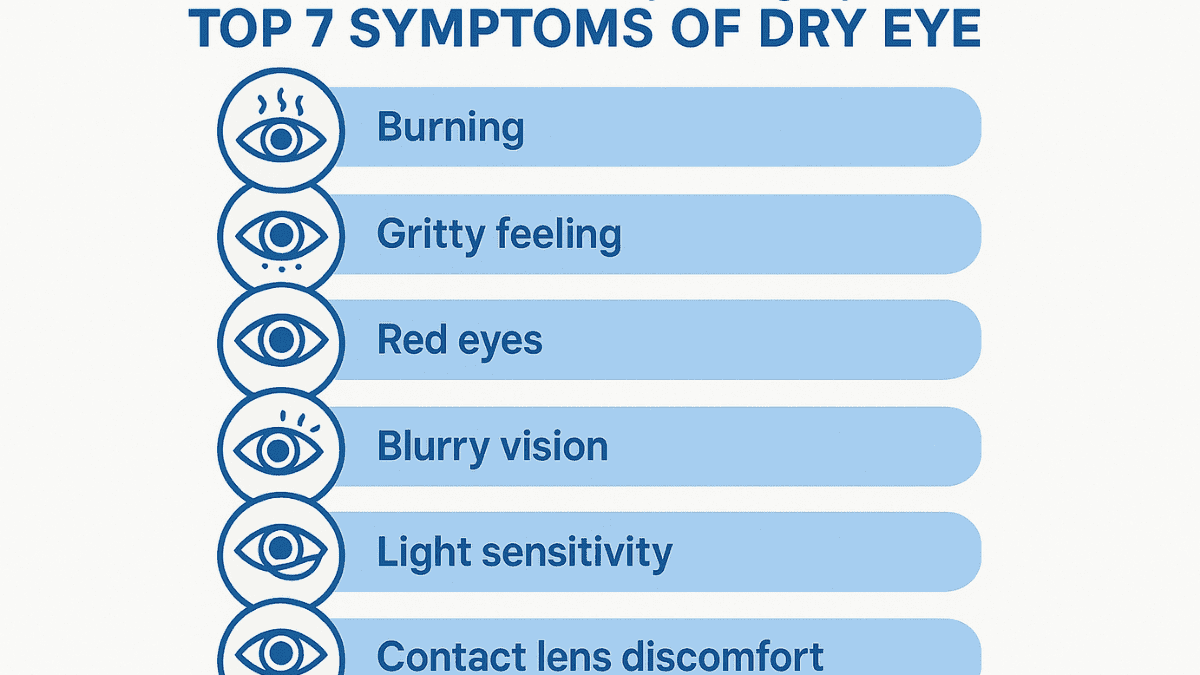
Look out for these telltale signs, as dry eyes include a range of sensations:
- A stinging, burning, or scratching sensation in your eyes.
- Feeling like there’s something gritty or sandy in your eye.
- Red, irritated eyes, which can be a sign of eye inflammation.
- Blurry vision that often comes and goes, especially after prolonged reading or screen time.
- Increased sensitivity to light (photophobia).
- Difficulty wearing contact lenses comfortably.
- Watery eyes, which seems counterintuitive, but it’s often your eyes trying to compensate for the dryness by producing an increased tear volume of poor-quality tears.
- Stringy mucus in or around the eyes.
If you’re experiencing several of these eye symptoms regularly, it’s a good idea to consult your eye doctor. An eye exam can help determine the underlying cause and the best course of treatment for your specific ocular surface disease. Ignoring these symptoms can sometimes lead to more severe dry eye problems or even an eye infection if the ocular surface is compromised.
What Causes Dry Eye?
Dry eye disease can have many different causes, often related to either decreased tear production or increased tear evaporation. Identifying the specific cause is important for effective management. Several risk factors can contribute to the development of this common eye condition.
Age
As we get older, our eyes naturally produce fewer tears; this is a primary reason for decreased tear production. That’s why dry eye becomes more common after age 50. Women, particularly after menopause due to hormonal changes, may experience dry eye symptoms more frequently than men of the same age group, affecting their tear glands.
Environmental Factors
Dry, windy climates can significantly increase tear evaporation from the eye’s surface. Spending a lot of time in air-conditioned or heated rooms, where dry air is prevalent, also contributes to this problem. Even prolonged staring at computer screens, smartphones, or other digital devices can reduce your blink rate, leading to incomplete spreading of the tear film and faster evaporation.
Medications
Certain medications can have side effects that reduce tear production. Common culprits include antihistamines used for allergies, decongestants for colds, some blood pressure medications (like diuretics and beta-blockers), antidepressants, and medications for Parkinson’s disease. If you suspect your medication is causing dry eye, discuss it with your doctor; do not stop any medication without medical advice.
Medical Conditions
Several medical conditions are associated with dry eye. Autoimmune disorders like Sjogren’s syndrome, where the immune system attacks moisture-producing glands including the lacrimal glands and salivary glands, are a significant cause of severe dry eyes. Rheumatoid arthritis and lupus can also affect tear production, leading to ocular surface disease. Other conditions including diabetes and thyroid problems (especially an overactive or underactive thyroid) can contribute to dry eye syndrome. Even conditions like graft-versus-host disease after a transplant can lead to severe dry eye.
Contact Lens Wear
While many people wear contact lenses without issue, for some, they can contribute to dry eye symptoms. Contact lenses can absorb some of the tear film, leading to dryness, or disrupt the natural spread of tears across the ocular surface. Proper lens care and choosing the right type of contact lens can mitigate some of these issues, but prolonged wear, especially in susceptible individuals, remains a risk factor for increased tear evaporation.
Eyelid Problems and Gland Dysfunction
The health of your eyelids and the glands within them, such as the meibomian glands, is crucial for a healthy tear film. Meibomian gland dysfunction (MGD) is a common condition where these glands, which produce the oily layer of the tear film, become blocked or don’t produce enough oil. This leads to a tear film that evaporates too quickly, a major cause of increased tear evaporation. Blepharitis, an inflammation of the eyelids, can also contribute to dry eye symptoms.
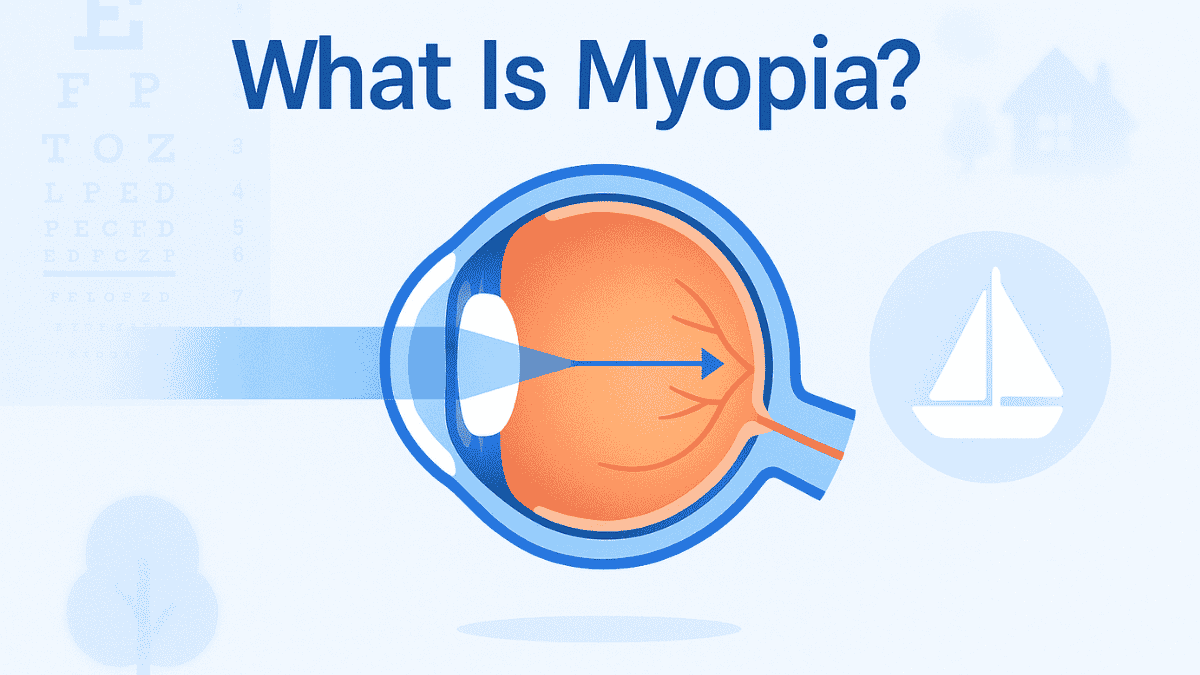
Eye Surgery and Other Factors
Certain types of eye surgery, such as laser eye surgery (e.g., LASIK) or other refractive surgeries, can temporarily or sometimes chronically cause dry eye. This is often due to nerve damage during the procedure, affecting tear production. Other factors include nutritional deficiencies (especially Vitamin A or omega-3 fatty acids), and allergic eye disease, which can cause inflammation and worsen dryness. High blood pressure or medications for it may also contribute.
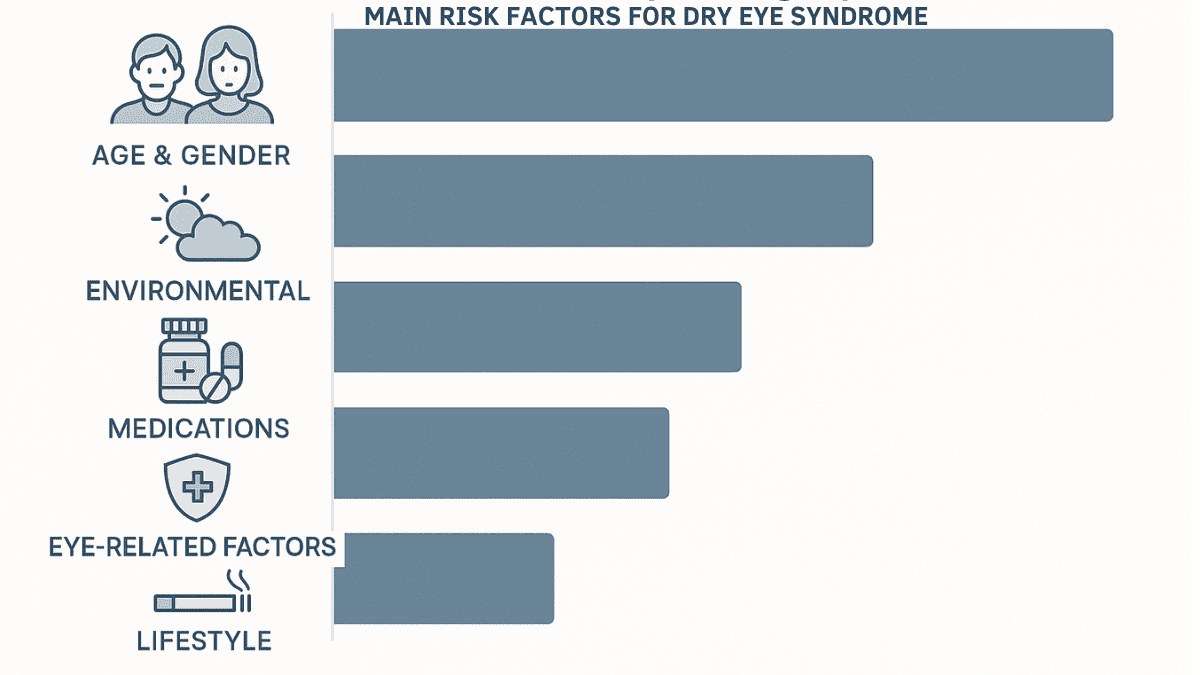
Here’s a table summarizing some common risk factors for dry eye:
| Category | Specific Risk Factors |
|---|---|
| Age & Gender | Being over 50; being female (especially post-menopausal). |
| Environmental | Dry air (wind, low humidity, air conditioning, heating); prolonged screen use. |
| Medications | Antihistamines, decongestants, diuretics, beta-blockers, antidepressants, some acne medications. |
| Medical Conditions | Sjogren’s syndrome, rheumatoid arthritis, lupus, diabetes, thyroid disorders, Parkinson’s disease, rosacea, allergic eye disease. |
| Eye-Related Factors | Contact lens wear, history of refractive surgery (laser eye surgery), meibomian gland dysfunction, blepharitis. |
| Lifestyle & Diet | Smoking, low intake of Vitamin A or omega-3 fatty acids. |
Home Remedies for Dry Eye Relief
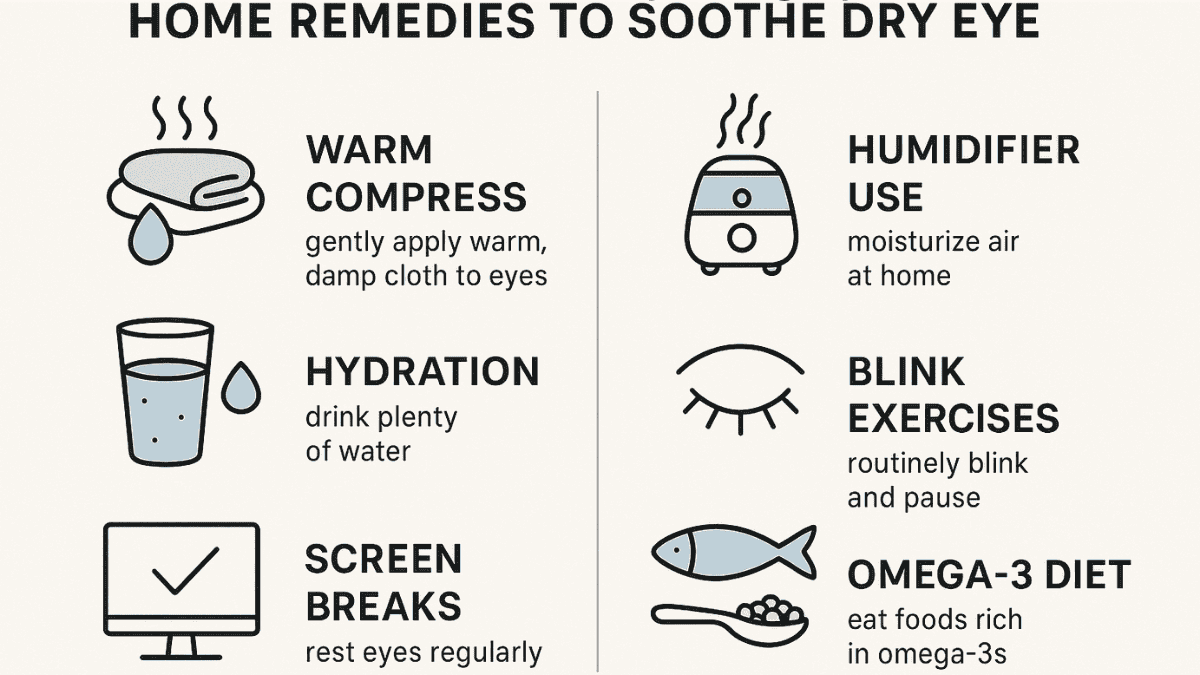
Before seeking medical treatments, many individuals find relief from dry eye symptoms through simple home remedies. These approaches can help improve tear quality and quantity, and protect the ocular surface. Consistent application of these remedies is often necessary to see sustained improvement.
Use a Warm Compress
Applying a warm, damp washcloth to your closed eyelids for 5-10 minutes can be very beneficial. This gentle heat helps to stimulate tear production and can also help unclog blocked meibomian glands, which produce the oily layer of the tear film that prevents rapid tear evaporation. Doing this once or twice a day can make a noticeable difference, especially for those with meibomian gland dysfunction.
Stay Hydrated
Overall body hydration plays a role in your ability to produce tears. Drinking plenty of water throughout the day helps your body, including your tear glands, function optimally to produce tears. Aim for 8-10 glasses of water daily, or more if you are active or in a hot, dry climate.
Take Screen Breaks
When concentrating on screens, people tend to blink less frequently, leading to increased tear evaporation. Follow the 20-20-20 rule: every 20 minutes, take a break and look at something 20 feet away for at least 20 seconds. This practice gives your eyes a chance to rest, re-moisten, and naturally spread the tear film through blinking.
Use a Humidifier
Adding moisture to the air with a humidifier can significantly reduce tear evaporation. This is especially helpful in dry climates or during winter when indoor heating creates dry air. Maintaining indoor humidity levels between 30-50% can help keep your eyes more comfortable.
Blink Exercises
Consciously blinking more often during prolonged visual tasks helps maintain a stable tear film. Gentle, full blinks ensure the tear film spreads evenly across the eye’s surface. Practice by closing your eyes slowly, pausing, then opening again, repeating throughout the day.
Dietary Adjustments
Including foods rich in omega-3 fatty acids may improve tear quality and reduce eye inflammation. Good sources include fatty fish like salmon, mackerel, and sardines, as well as flaxseeds, chia seeds, and walnuts. A balanced intake is important as some vegetable oils high in omega-6 can be pro-inflammatory. Consult a healthcare provider or nutritionist for personalized advice.
Over-the-Counter Treatments for Dry Eye
If home remedies aren’t enough, several over-the-counter (OTC) treatments are available to supplement natural tear production, reduce tear evaporation, or address inflammation. These options are convenient and effective for managing mild to moderate dry eye disease.
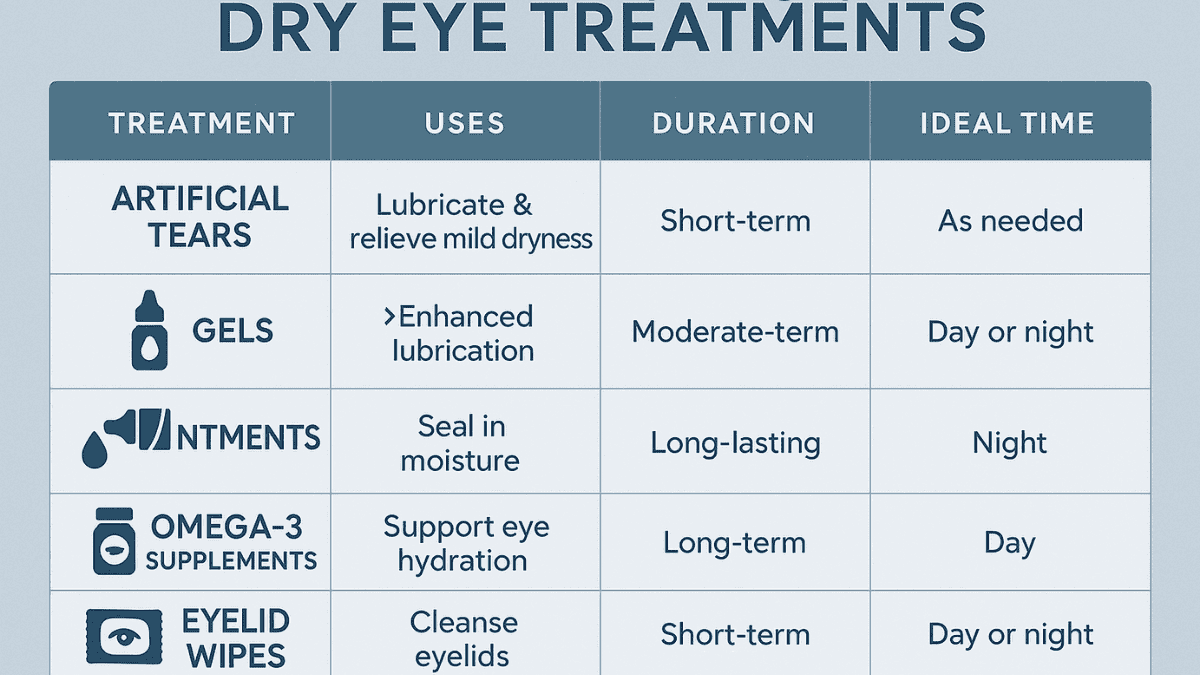
Artificial Tears
Artificial tears are eye drops designed to mimic your natural tears, providing lubrication and moisture to the ocular surface. They are often the first line of treatment for dry eye. Various formulations exist, differing in viscosity and preservatives. Some replenish the aqueous fluid layer, while others contain lipids to stabilize the oily layer and reduce evaporation. Preservative-free artificial tears are recommended for frequent use (more than four times daily) to avoid irritation.
Eye Gels and Ointments
For more persistent or severe dry eyes, thicker lubricating eye gels and ointments offer longer-lasting relief. With higher viscosity, they remain on the eye surface longer but may cause temporary blurring of vision. They are best used before bedtime to provide overnight comfort, especially helpful for those who wake up with dry, irritated eyes.
Omega-3 Supplements
Research suggests that oral omega-3 fatty acid supplements can help improve dry eye symptoms by reducing inflammation and enhancing the quality of the meibomian gland oil. These supplements support the lipid layer of the tear film, reducing tear evaporation. Common sources include fish oil and flaxseed oil. Discuss supplementation with your doctor, especially if you take other medications or have health conditions.
Eyelid Wipes and Cleansers
For dry eye linked to eyelid inflammation (blepharitis) or meibomian gland dysfunction, specialized eyelid wipes or cleansers can help. These remove debris, bacteria, and excess oils from the eyelid margins, improving gland function and reducing inflammation. Maintaining regular eyelid hygiene is an important part of managing these dry eye symptoms.
When to See a Doctor for Dry Eye
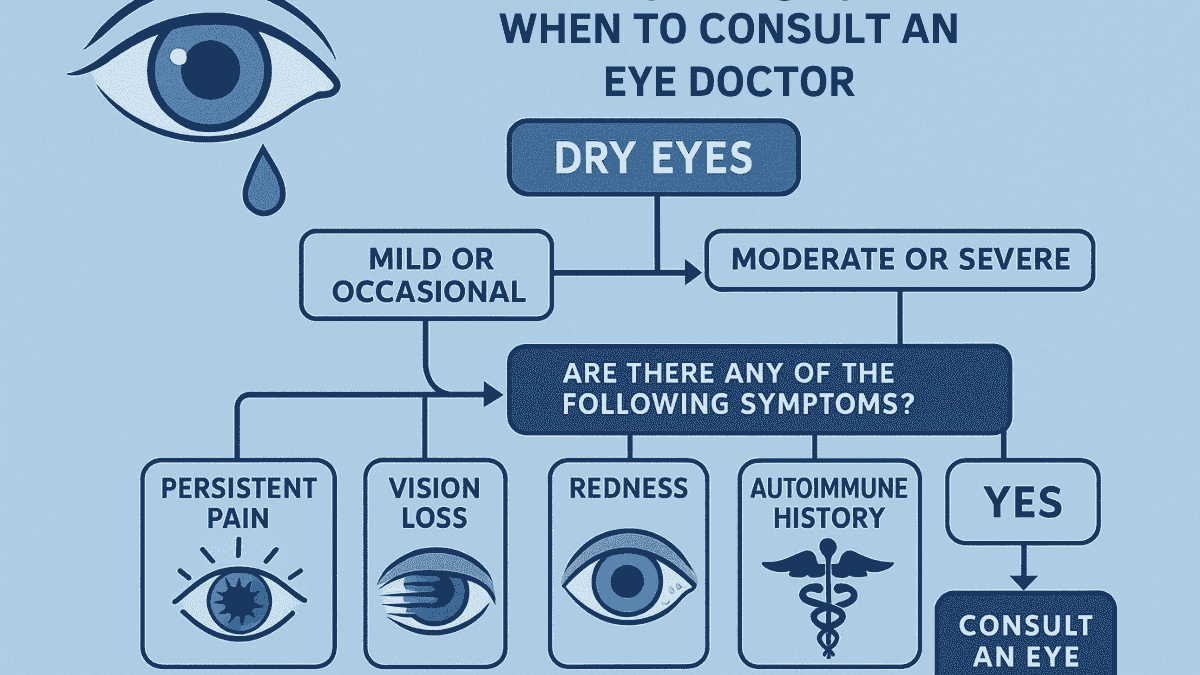
While many cases of dry eye can be managed effectively with home remedies and over-the-counter treatments, professional medical advice is necessary in some situations. An eye exam by an optometrist or ophthalmologist can accurately diagnose the cause and severity of your dry eye disease, which is crucial for developing an effective treatment plan, especially for persistent or severe dry eyes.
Schedule an appointment with your eye care professional if you experience:
- Severe symptoms significantly impacting daily life or not improving with home treatments and artificial tears.
- Noticeable decrease in vision or persistent eye pain, which may indicate a more serious problem.
- Extremely red or swollen eyes, possibly signaling significant inflammation or infection.
- A history of autoimmune disorders like Sjogren’s syndrome or rheumatoid arthritis, requiring specialized dry eye management.
- Suspected dry eye symptoms caused by a new medication.
During a dry eye exam, your doctor may perform tests such as tear breakup time, Schirmer test for tear production, and an examination of the eyelids and meibomian glands. These results guide personalized treatment, which could include prescription medications or in-office procedures for advanced ocular surface disease. The Mayo Clinic provides reliable information on what to expect during these assessments.
Advanced Treatments for Chronic Dry Eye
For individuals suffering from chronic or severe dry eye disease that does not respond adequately to conservative measures, more advanced treatments are available. These options target the underlying causes of dry eye, such as insufficient tear production from the lacrimal glands or excessive tear evaporation caused by meibomian gland dysfunction. An eye care specialist can assess your condition and determine if these treatments are appropriate for you.
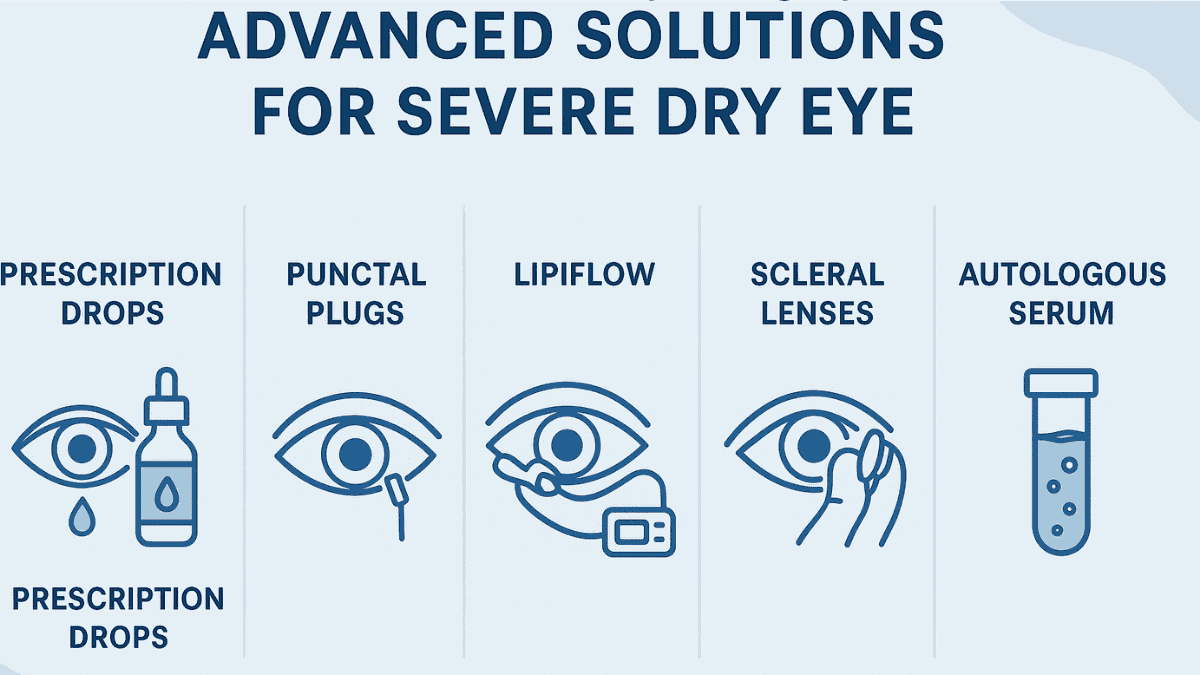
Prescription Eye Drops
Several types of prescription eye drops help manage chronic dry eye. Medications like cyclosporine (e.g., Restasis) and lifitegrast (e.g., Xiidra) reduce inflammation on the eye’s surface, promoting increased natural tear production over time. Corticosteroid eye drops may be prescribed short-term to quickly reduce significant eye inflammation linked to severe dry eye syndrome.
Punctal Plugs
If tears drain too quickly, your doctor may recommend punctal plugs—tiny, biocompatible devices inserted into the tear ducts (puncta) in your eyelids. By blocking these drainage channels partially or completely, punctal plugs help retain natural and artificial tears longer on the eye’s surface, improving lubrication and reducing dry eye symptoms.
LipiFlow Thermal Pulsation
LipiFlow is an in-office treatment for meibomian gland dysfunction (MGD), a major cause of evaporative dry eye. It applies controlled heat and gentle pressure to the inner eyelids to liquefy and express clogged oils from the meibomian glands. Improving gland function helps restore the oily layer of the tear film, stabilizing tears and reducing evaporation.
Other Specialized Treatments
In cases of very severe dry eye, other treatments may be considered. These can include scleral lenses, which are large-diameter gas permeable contact lenses that vault over the cornea and rest on the white part of the eye (sclera), creating a reservoir of fluid over the ocular surface. Autologous serum eye drops, made from the patient’s own blood, can also be used as they contain growth factors and nutrients beneficial for healing the eye’s surface. These options are typically reserved for complex cases of ocular surface disease.
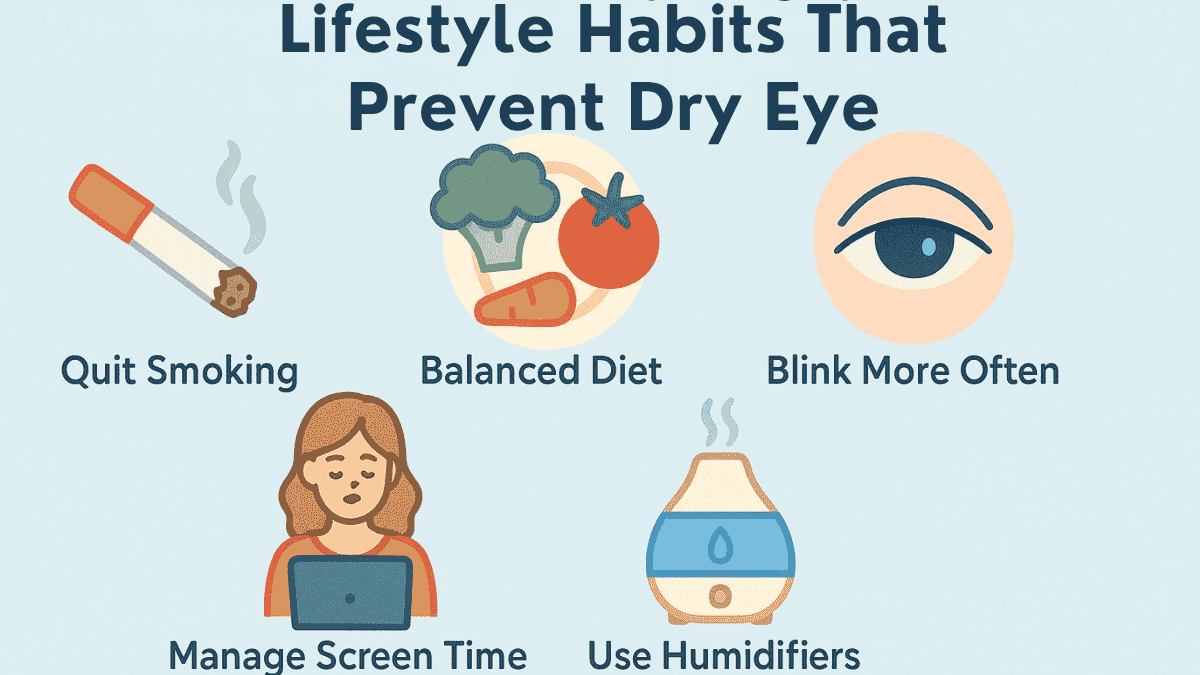
Lifestyle Changes to Prevent Dry Eye
Making a few thoughtful adjustments to your daily routine and environment can significantly contribute to preventing dry eye symptoms or reducing their frequency and severity. These lifestyle changes often focus on minimizing tear evaporation and supporting overall eye health. Proactive eye care can make a substantial difference in maintaining comfortable, healthy eyes.
Wear Sunglasses Outdoors
Protect your eyes from environmental elements like wind, sun, and dry air by wearing sunglasses, preferably wraparound styles. These help reduce tear evaporation, especially in windy conditions or bright sunlight, which can worsen dry eye.
Quit Smoking
Tobacco smoke irritates eyes and worsens dry eye symptoms. Smoking damages the meibomian glands and alters tear film composition. Quitting improves overall eye health and reduces discomfort.
Eat a Balanced Diet
A nutrient-rich diet supports eye health. Foods high in vitamin A (carrots, sweet potatoes, leafy greens) and omega-3 fatty acids (salmon, flaxseeds, walnuts) help maintain a healthy tear film and reduce inflammation. Balance fatty acid intake for best results.
Blink More Often
During activities like reading or screen use, people blink less, increasing dryness. Consciously blink fully and regularly to spread tears and keep eyes moist and clear.
Optimize Your Environment
Take steps to modify your environment to be more eye-friendly. Avoid direct exposure to airflow from fans, air conditioners, or heaters. Use a humidifier to add moisture to dry indoor air, especially during winter months or in arid climates. Position your computer screen below eye level; this can help reduce eyelid opening and slow down tear evaporation.
Manage Screen Time
Prolonged screen use is a major contributor to evaporative dry eye due to reduced blink rates. Implement regular breaks, such as the 20-20-20 rule: every 20 minutes, look away from your screen at an object 20 feet away for at least 20 seconds. This helps your eyes to relax and re-lubricate. Adjust screen brightness and contrast to comfortable levels and consider using a matte screen filter to reduce glare, which can also cause eye strain and dryness. Proper eye care when using digital devices is crucial.
Conclusion
Dry eye is a common condition often linked to specific risk factors or medical conditions, but it doesn’t have to control your daily comfort or vision quality. With the right mix of home remedies, proper use of artificial tears or other over-the-counter treatments, and helpful lifestyle changes, most people find significant relief from dry eye symptoms. Understanding the role of tear production by the tear glands and problems like increased tear evaporation is the crucial first step.
Your eyes are precious, and addressing discomfort early is key to maintaining a healthy ocular surface. Don’t hesitate to consult an eye care professional if you experience persistent dry eye, especially if it’s severe or linked to conditions like rheumatoid arthritis or Sjogren’s syndrome. A thorough eye exam can detect issues such as meibomian gland dysfunction or lacrimal gland problems, enabling effective management of your dry eye or ocular surface disease.
With patience, consistent care, and the right approach—which may include simple adjustments or managing underlying conditions like high blood pressure or effects from laser eye surgery—you can regain clear and comfortable vision. Proactive management of dry eye syndrome can greatly enhance your quality of life. Remember to consider every aspect, from the aqueous fluid in your tears to the health of your meibomian glands, for comprehensive eye care.
Dry eye syndrome is a condition where your eyes don’t produce enough tears or the tears evaporate too quickly, causing irritation and discomfort.
Burning, stinging, gritty sensation, redness, and blurry vision are common dry eye symptoms.
Causes include aging, medications, autoimmune diseases, environmental factors, and screen use.
Prolonged screen use reduces blink rate, leading to tear film instability and evaporation.
Yes, insufficient hydration reduces tear production and worsens symptoms.
Yes, especially preservative-free types that mimic natural tear composition.
MGD is a blockage or abnormality in glands that produce the oily tear layer, causing rapid evaporation.
Yes, unstable tear film can lead to intermittent blurry vision and eye fatigue.
If symptoms persist, worsen, or include pain or vision changes, consult a specialist.
Yes, it can be linked to conditions like Sjögren’s, diabetes, thyroid disorders, and lupus.
Omega-3s reduce inflammation and improve tear quality by enhancing the oil layer.
Yes, it’s often worse in winter or during allergy seasons due to dry air and inflammation.

For some, yes—contacts can absorb tear film and limit oxygen flow.
LipiFlow is a device that heats and massages eyelids to clear meibomian glands.
Yes. Staying hydrated, blinking often, and using humidifiers can help.