Imagine a laser eye surgery that corrects your vision without any surgical blades or manual handling of the eye’s surface. This is the promise of TransPRK surgery, a sophisticated ‘no-touch’ procedure revolutionizing the path to clearer sight. If you are exploring options to improve vision and reduce dependence on glasses or contact lenses, understanding TransPRK is an important step.
This advanced surface ablation technique, also known as Transepithelial Photorefractive Keratectomy, offers a distinct approach compared to other laser eye surgeries. Learning about its specifics can help you determine if TransPRK aligns with your visual needs and lifestyle. This guide will cover what makes TransPRK stand out.
Table of Contents
What Exactly is TransPRK?
TransPRK stands for Transepithelial Photorefractive Keratectomy, a name that reveals much about its method. Photorefractive Keratectomy (PRK) is a foundational type of laser eye surgery. The “Transepithelial” prefix signifies the laser works directly through the epithelium, the cornea’s outermost protective layer.
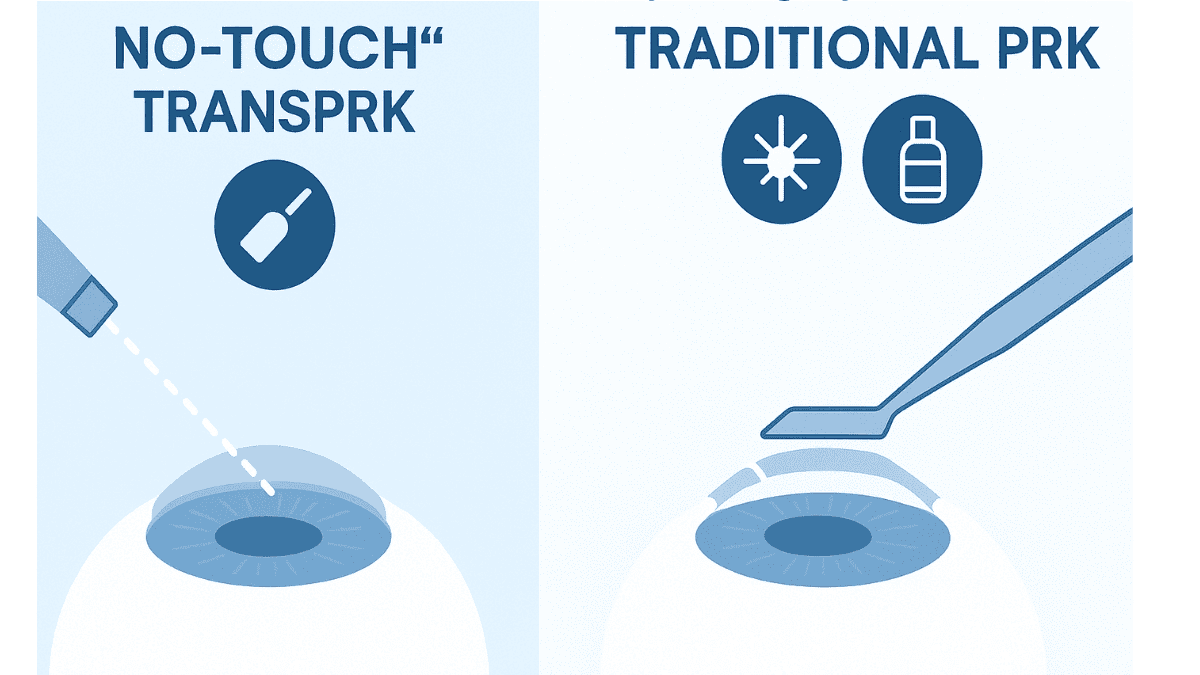
What truly distinguishes TransPRK is its nature as a ‘no-touch’ or ‘all-laser’ advanced surface ablation. During this single step procedure, no surgical instruments or diluted alcohol solutions are used to manually remove the epithelium. Instead, an excimer laser performs both the epithelial removal and the subsequent corneal reshaping to correct refractive errors.
This integrated approach differs significantly from traditional PRK, where epithelial removal is manual. It also contrasts with LASIK surgery, which necessitates creating a corneal flap. TransPRK avoids a flap entirely, categorizing it as an advanced surface treatment that many find appealing.
Understanding the “No-Touch” Aspect of TransPRK
The “no-touch” characteristic is central to TransPRK’s appeal. The laser executes two critical functions in one seamless operation. It first ablates the epithelium and then immediately reshapes the underlying corneal stroma to correct vision issues like myopia or hyperopia.
This single step procedure is meticulously managed by advanced laser systems, such as the Schwind Amaris laser, informed by detailed ocular scans. This all-laser approach, sometimes referred to conceptually as a ‘touch lazer’ due to the laser’s direct and precise interaction, can feel less intrusive for patients. Research suggests this laser-driven epithelial removal results in an exceptionally smooth corneal surface, potentially aiding more uniform and rapid epithelial regrowth compared to older methods.
Furthermore, the reliance on technology like the Amaris laser minimizes human variables in epithelial removal. This reduces the possibility of minor inconsistencies associated with manual techniques. Such precision is a hallmark of modern laser refractive surgery developments.
How Does the TransPRK Procedure Work? Step-by-Step
Knowing what happens during any medical procedure can make you feel more comfortable. TransPRK, while advanced, follows a clear path. It all begins well before you arrive at the surgery room.
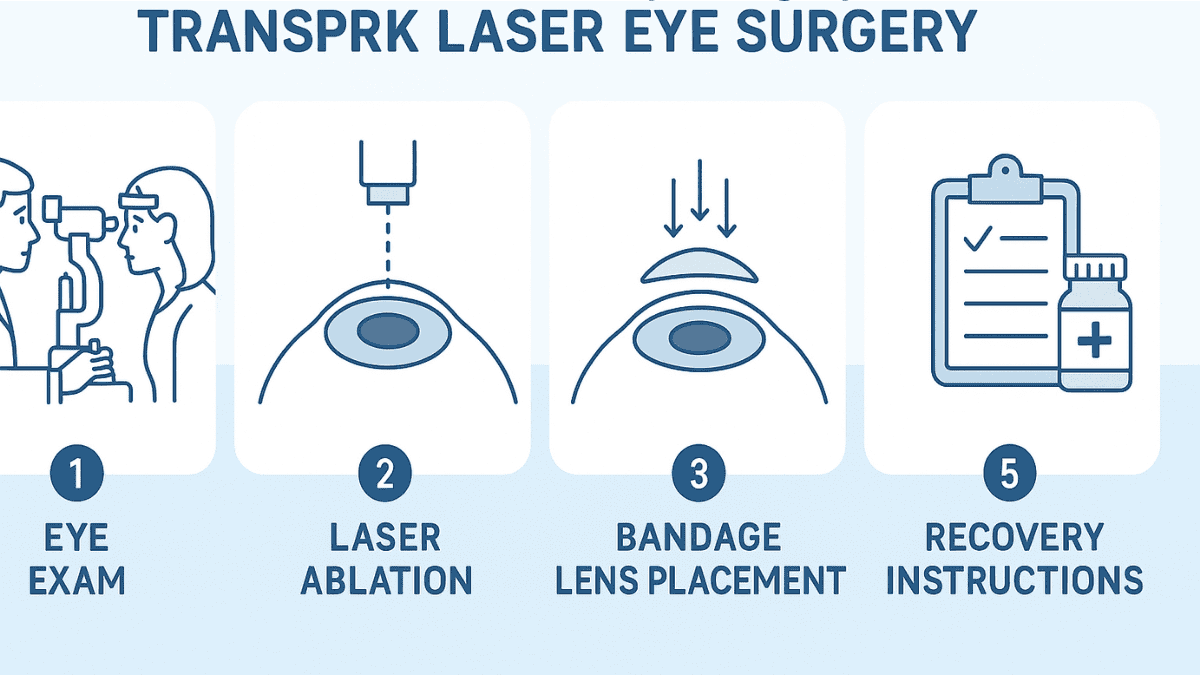
Pre-Procedure Preparations
Your path to TransPRK surgery starts with a comprehensive eye consultation. During this visit, your ophthalmologist will evaluate your vision, accurately measure your prescription for any refractive errors, and thoroughly assess your ocular health. Corneal thickness, a critical parameter for any laser refractive procedure, will also be precisely measured, especially if you are among those with a thin cornea
This detailed examination is crucial for determining your suitability for TransPRK, as not all individuals are ideal candidates for every type of laser vision correction. If you regularly use contact lenses, you will typically need to discontinue the contact lens worn for a specified period before both your consultation and the surgery. This pause allows your cornea to revert to its natural contour, vital for obtaining the most accurate measurements needed to correct refractive issues effectively.
Your doctor will provide explicit instructions regarding this and other preparatory steps. Understanding nasil bir (what kind of) outcome to expect and addressing all queries during the eye consultation is important. This helps set realistic expectations for the TransPRK surgery and subsequent visual recovery.
The Day of the Surgery
Upon arrival at the clinic for your TransPRK procedure, the medical team will prepare you for the surgery. Anesthetic eye drops will be administered to numb your eyes completely, ensuring you do not feel pain during the laser application. You might sense slight pressure, but the treatment itself is painless.
You will then recline beneath the sophisticated laser system. A small instrument, an eyelid speculum, will be carefully positioned to hold your eyelids open. This precaution prevents blinking while the laser is active, which is essential for the precision of this step procedure.
The Laser Treatment
You will be instructed by the surgeon to focus on a target light, which aids in maintaining optimal eye alignment and stability. Modern laser platforms for TransPRK, prominently including the Schwind Amaris laser, feature advanced eye-tracking systems. These trackers compensate for minute, involuntary eye movements, directing laser pulses with exceptional accuracy to the surface cornea.
The laser then executes the treatment. It begins by gently vaporizing the epithelium, the thin outer layer. Immediately following this, the same laser reshapes the corneal stroma beneath to correct your specific vision prescription.
The entire laser application is remarkably swift, typically completed in under a minute per eye. Some clicking sounds or a faint odor may be noticeable; these are normal byproducts of the laser vaporizing corneal tissue with high precision, a key aspect of this single step technique.
Post-Laser Care
After the laser treatment concludes, the surgeon will place a special contact lens on your eye. This is a transparent bandage lens, and this special contact lens worn over the treated area serves to protect the surface cornea. It also enhances comfort and supports the epithelial regeneration process.
You will receive prescriptions for several types of eye drops. Typically, these include antibiotics to guard against infection and anti-inflammatory drops to facilitate healing and minimize swelling. Detailed guidance on the use of these drops, alongside other post-operative care instructions, will be provided for the recovery period following the transepithelial photorefractive keratectomy.
You will then be able to return home, though arranging for someone to drive you is necessary. It’s important to note that, unlike some older PRK techniques, modern TransPRK does not involve the use of diluted alcohol for epithelial removal, which contributes to its refined healing profile. Adherence to post-operative instructions is vital for a smooth recovery and optimal outcome to improve vision.
Who is a Good Candidate for TransPRK?
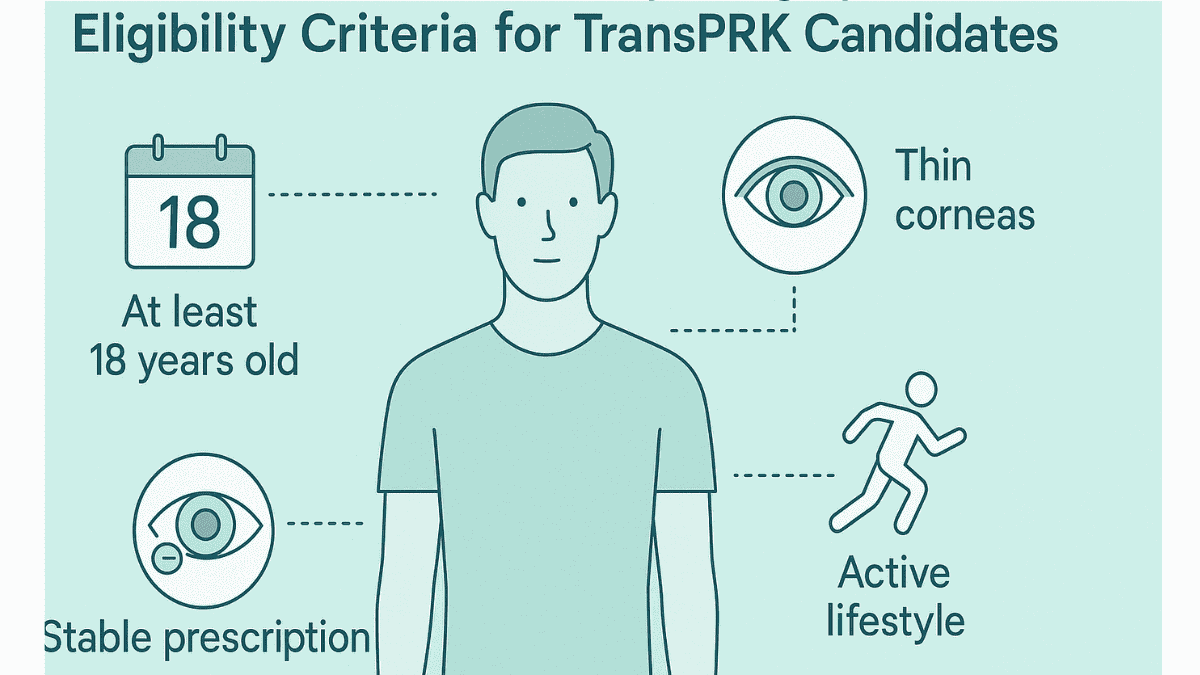
Determining suitability for TransPRK involves several considerations. Candidates are generally 18 years or older, sometimes 21, to allow for prescription stability for at least one year before undergoing any laser refractive surgery. A stable prescription is a fundamental requirement for predictable outcomes.
TransPRK effectively addresses common refractive errors such as myopia, hyperopia, and astigmatism. It can correct a wide range of prescriptions, including some instances of yüksek numaralara (high prescriptions), though your surgeon will verify if your specific refractive needs are within the optimal treatment zone. The procedure is formulated to correct refractive issues with precision.
A notable advantage of TransPRK is its suitability for individuals with thin corneas. As a surface ablation, it avoids creating a corneal flap, thereby conserving more corneal tissue. This makes TransPRK a viable option for some who were not candidates for LASIK due to having a korneası ince (thin cornea).
Furthermore, those whose cornea surface is steeper than normal may also find TransPRK beneficial, though this needs careful assessment. Lifestyle also plays a role; individuals in contact sports or professions with a high risk of eye trauma often prefer TransPRK. The absence of a corneal flap eliminates flap-related risks from direct impact.
Patients with pre-existing dry eyes may also benefit, as some studies suggest TransPRK could result in less severe or prolonged dry eye symptoms compared to LASIK. However, certain conditions can make TransPRK unsuitable. These include severe dry eye syndrome, autoimmune diseases impacting healing, conditions like keratoconus, or active ocular infections.
It is also important to consider overall eye health. For example, conditions like advanced age-related macular degeneration might influence the decision or expected outcome of any elective vision correction. A thorough eye health evaluation during your eye consultation is essential to ascertain if TransPRK is the right choice for you and to discuss how TransPRK surgery aims to improve vision safely.
Advantages of Choosing TransPRK

TransPRK, also known as transepithelial photorefractive surgery, offers compelling benefits, positioning it as a strong option in laser vision correction. Its flap-less and ‘no-touch’ characteristics are primary attractions for many individuals. Let’s examine these advantages.
No Flap, No Flap-Related Complications
The most prominent benefit over LASIK is the absence of a corneal flap. As an advanced surface ablation procedure, TransPRK does not involve cutting a flap. This inherently removes all risks tied to corneal flaps, such as displacement, wrinkles, or under-flap inflammation (diffuse lamellar keratitis).
This absence of flap-related concerns offers considerable reassurance for many patients. It simplifies one aspect of the surgical process and recovery. The focus remains on the healing of the surface cornea itself.
Truly “No-Touch” Technique
The entire process of epithelial removal and corneal reshaping is performed by the excimer laser, a true ‘touch lazer’ application. For patients apprehensive about surgical instruments near their eyes, this automated aspect can lessen anxiety. This all-laser method minimizes mechanical handling of the corneal surface, potentially being gentler.
The Schwind Amaris laser system, for instance, exemplifies this technology. The precision of such lasers strengthens the effectiveness of the ‘no-touch’ approach. All associated patented technologies typically have their rights reserved by the developers, reflecting the innovation involved.
Corneal Stability
By forgoing a flap, TransPRK maintains more of the cornea’s inherent structural integrity. The cornea remains stronger as it does not undergo a significant lamellar incision. Many surgeons assert this contributes to superior long term biomechanical stability of the cornea.
This enhanced stability is especially valuable for individuals with corneas that are ince olan (thin) from the outset. It’s also crucial for those in professions or lifestyles with increased risk of eye trauma. This focus on long term corneal health is a key benefit.
Potentially Faster Epithelial Healing (compared to traditional PRK)
While TransPRK’s initial recovery may involve more discomfort than LASIK, it often features more comfort and quicker visual recovery than traditional photorefractive keratectomy. The laser’s precision in epithelial removal creates a very smooth foundation. This smoothness encourages new epithelial cells to regenerate more uniformly and rapidly.
Studies indicate this can lead to quicker visual clarification and reduced discomfort compared to older PRK techniques. This refined healing is a direct result of the advanced surface treatment. This is a step procedure that shows progress.
Good for Active Lifestyles and Specific Professions
For individuals whose occupations or hobbies carry a risk of facial or ocular impact, such as contact sports or emergency services, TransPRK is frequently recommended. Without a corneal flap, concerns about flap dislodgement or tears from injury, even years post-surgery, are eliminated. This resilience makes TransPRK a sound choice for active people who wish to improve vision.
What to Expect During TransPRK Recovery
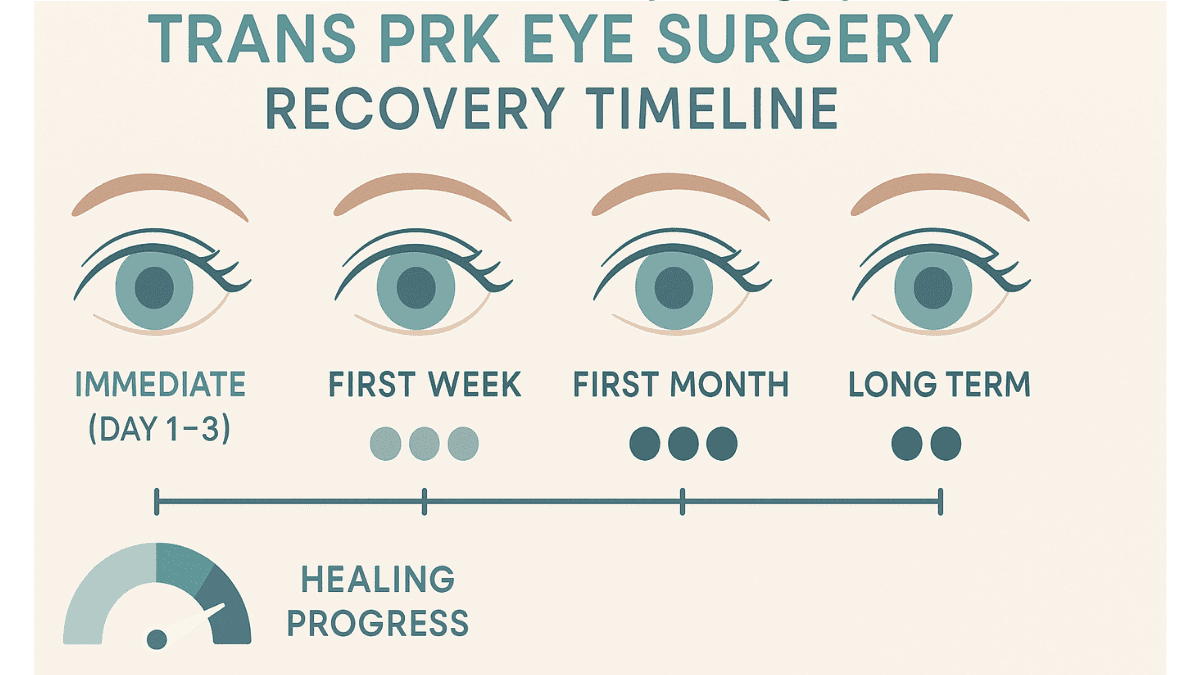
The recovery from TransPRK, a form of transepithelial photorefractive keratectomy, differs somewhat from other laser eye surgeries. Understanding the typical stages is helpful. Patience is a virtue as your eyes heal and vision stabilizes over the long term.
Immediately After Surgery
Directly following your TransPRK surgery, expect your vision to be noticeably blurry. Light sensitivity, a foreign body sensation, and excessive tearing are common initial reactions. As anesthetic drops wear off, some discomfort or pain is likely.
This discomfort peaks during the first 2 to 3 days while the epithelium heals. Your doctor can prescribe pain relief and provide management advice. The special contact lens worn (bandage lens) remains on the eye to protect it during this critical healing phase.
The First Week
The primary focus during the first week post-surgery is the regeneration of your corneal epithelium. This outer layer must regrow over the treated surface cornea. Vision will begin to improve as it heals, but fluctuations between clarity and blurriness are normal.
Discomfort typically lessens considerably once epithelial closure occurs, usually within 3 to 5 days. Your surgeon will remove the bandage contact lens at a follow-up visit upon confirming sufficient surface healing. Strict adherence to prescribed antibiotic and anti-inflammatory eye drops is crucial.
Subsequent Weeks and Months
Vision continues to sharpen and achieve stability in the ensuing weeks and months. While good vision is often experienced within one or two weeks, achieving your final optimal vision can take several weeks to three months. This period can sometimes be longer for those with yüksek numaralara (high prescriptions) or a cornea that is normalden daha dik (steeper than normal).
Steroid eye drops will be required for a period, crucial for managing the healing response and preventing corneal haze. The duration of steroid use varies. It is imperative to follow your doctor’s instructions and attend all follow-up appointments for the best long term results.
Protecting your eyes from strong sunlight with UV-blocking sunglasses and avoiding eye rubbing are also important during this period. You will gradually resume normal activities, with your surgeon providing a specific timeline for each. This careful management supports the success of the advanced surface procedure.
Potential Risks and Side Effects of TransPRK
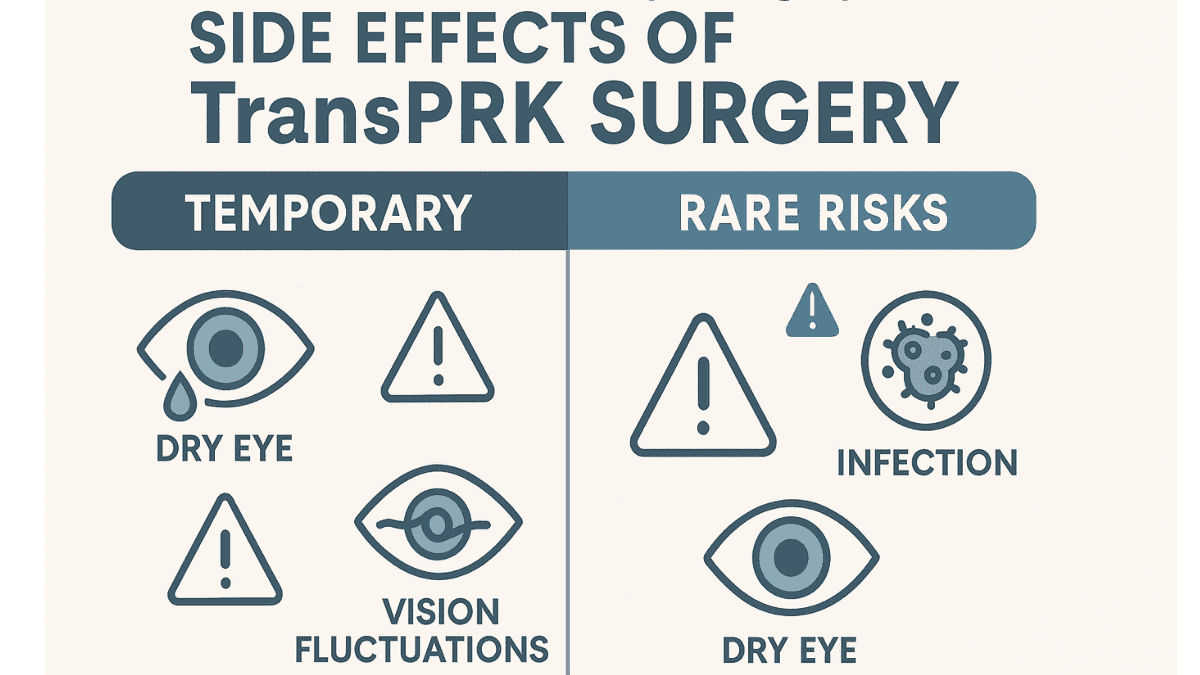
Any surgical intervention, including TransPRK surgery, carries potential risks and side effects. Serious complications are infrequent with experienced surgeons and advanced technology like the Schwind Amaris laser. However, awareness is important for an informed decision about this laser refractive surgery.
Common, generally temporary, side effects may include the following items.
- Pain or discomfort: Most pronounced in the initial days post-surgery, manageable with medication and the bandage lens worn.
- Blurry or fluctuating vision: Normal during healing, gradually improving over time.
- Light sensitivity (photophobia): Increased sensitivity to light for a period; sunglasses offer relief.
- Dry eyes: A frequent side effect of many laser eye surgeries, including TransPRK; usually temporary and managed with lubricating drops. Some individuals might experience more persistent dry eyes.
- Halos or glare: Seeing halos or starbursts around lights, particularly at night; typically diminishes as healing progresses.
- Less common, yet more serious, risks to discuss with your surgeon include these points.
- Corneal haze: A subtle corneal clouding during healing, more likely with higher prescriptions. Modern lasers, medications like Mitomycin C (if used), and steroid drops minimize this. If haze develops, it is usually mild and transient, but rarely it can affect vision. Sometimes, phototherapeutic keratectomy (PTK) techniques can be considered for significant, persistent haze, although this is rare.
- Infection: Extremely rare, with prescribed antibiotic eye drops significantly reducing this risk.
- Delayed epithelial healing: The surface layer occasionally takes longer to regenerate than average; your doctor will monitor this.
- Over or under-correction: The laser may correct vision more or less than intended. Minor variations are not unusual, but significant deviations might necessitate glasses, contacts, or a later enhancement procedure to fully correct refractive errors.
- Regression: A partial return of the refractive error over time can occur in some cases, a possibility with other laser eye procedures too.
- This list is not comprehensive. A thorough discussion about all potential risks with your surgeon during the eye consultation is essential. They will explain how these risks relate to your specific circumstances and the preventive measures taken.
TransPRK vs. Other Laser Eye Procedures: A Quick Look
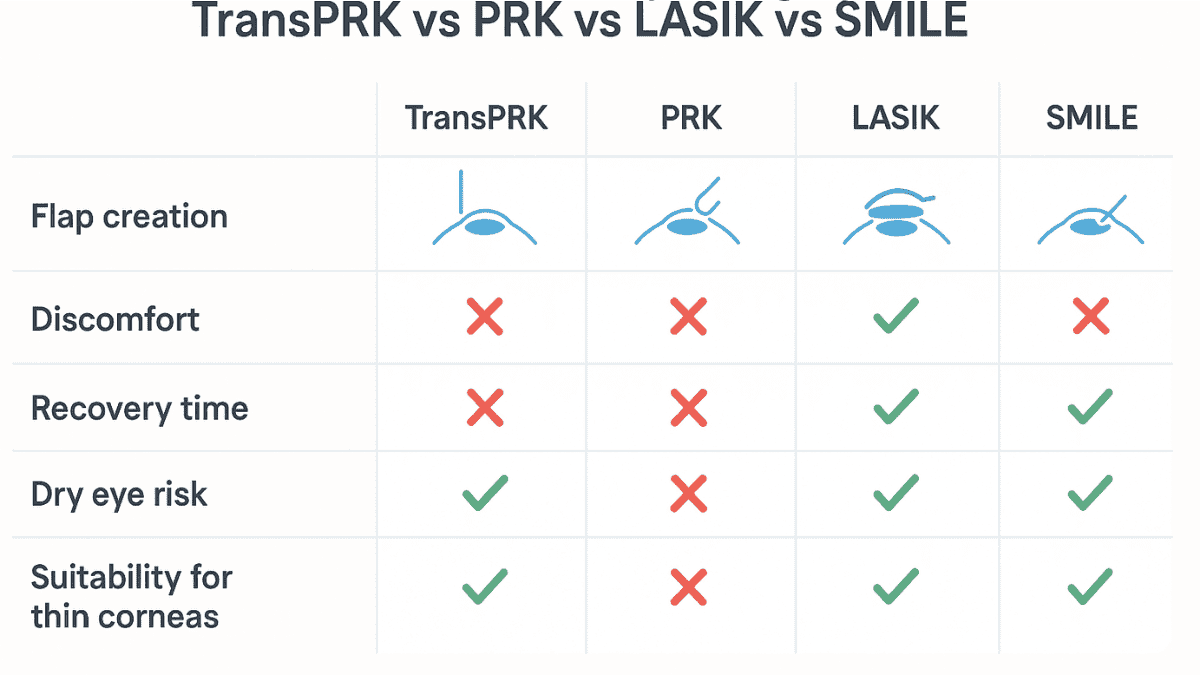
Many wonder how TransPRK, also known as transepithelial photorefractive keratectomy, compares to other laser vision correction methods. Each laser refractive surgery has specific strengths, suiting different eye conditions and patient needs. Understanding these distinctions facilitates a more productive discussion with your doctor about how to improve vision.
TransPRK vs. Traditional PRK
Both TransPRK and traditional photorefractive keratectomy (PRK) are surface cornea ablation techniques that reshape the cornea after epithelial removal, without flap creation. The primary difference lies in the method of epithelial removal. In traditional PRK, surgeons may use a brush, blade, or a diluted alcohol solution for manual cell removal.
Conversely, TransPRK employs an excimer laser for this task in a single step, ‘no-touch’ fashion. This laser-driven removal in the TransPRK step procedure is thought to create a smoother corneal bed. This potentially leads to slightly faster healing and less discomfort than some older PRK methods, though final visual outcomes are generally comparable once healing is complete.
TransPRK vs. LASIK/Femto-LASIK
LASIK (Laser-Assisted In Situ Keratomileusis) involves creating a thin corneal flap, which is lifted for laser reshaping and then repositioned. Femto-LASIK utilizes a femtosecond laser for more precise flap creation. LASIK’s main appeal is often faster visual recovery and minimal initial discomfort.
However, the flap introduces risks like dislocation or inflammation. TransPRK, being flap-less, bypasses these specific flap-related complications. It is also favored for thinner corneas (korneası ince olan) as it conserves more tissue, and some reports suggest a potentially lower risk of exacerbating dry eyes.
TransPRK vs. SMILE
SMILE (Small Incision Lenticule Extraction) is another advanced, minimally invasive option. A femtosecond laser creates a lenticule (a small, lens-shaped piece of tissue) within the cornea, which is then removed via a tiny incision. This reshapes the cornea and corrects vision, primarily myopia and astigmatism.
Like TransPRK, SMILE is flapless, a significant benefit. SMILE often provides rapid recovery, similar to LASIK. The choice between TransPRK and SMILE depends on factors like your prescription, corneal details (e.g. if it is normalden daha dik, meaning steeper than normal), and surgeon expertise. This makes the eye consultation critical.
This table offers a simplified comparison of these laser refractive options:
| Feature | TransPRK | Traditional PRK | LASIK/Femto-LASIK | SMILE |
|---|---|---|---|---|
| Flap Created | No | No | Yes | No (lenticule removal) |
| Epithelial Removal | Laser (no-touch) | Manual/Diluted Alcohol | N/A (under flap) | N/A (lenticule within stroma) |
| Initial Discomfort | Moderate | Moderate to High | Low | Low to Moderate |
| Visual Recovery Speed | Slower (days to weeks) | Slower (days to weeks) | Fast (hours to days) | Fast (hours to days) |
| Dry Eye Risk | Potentially Lower | Moderate | Potentially Higher | Potentially Lower |
| Good for Thin Corneas (ince olan) | Yes | Yes | Sometimes limited | Yes (to an extent) |
| Flap Complications Risk | None | None | Possible | None |
These are general comparisons. The optimal laser refractive surgery for you will depend on many personal factors and a thorough evaluation of your kornea yüzeyi (cornea surface) and overall eye health.
Preparing for Your TransPRK Journey
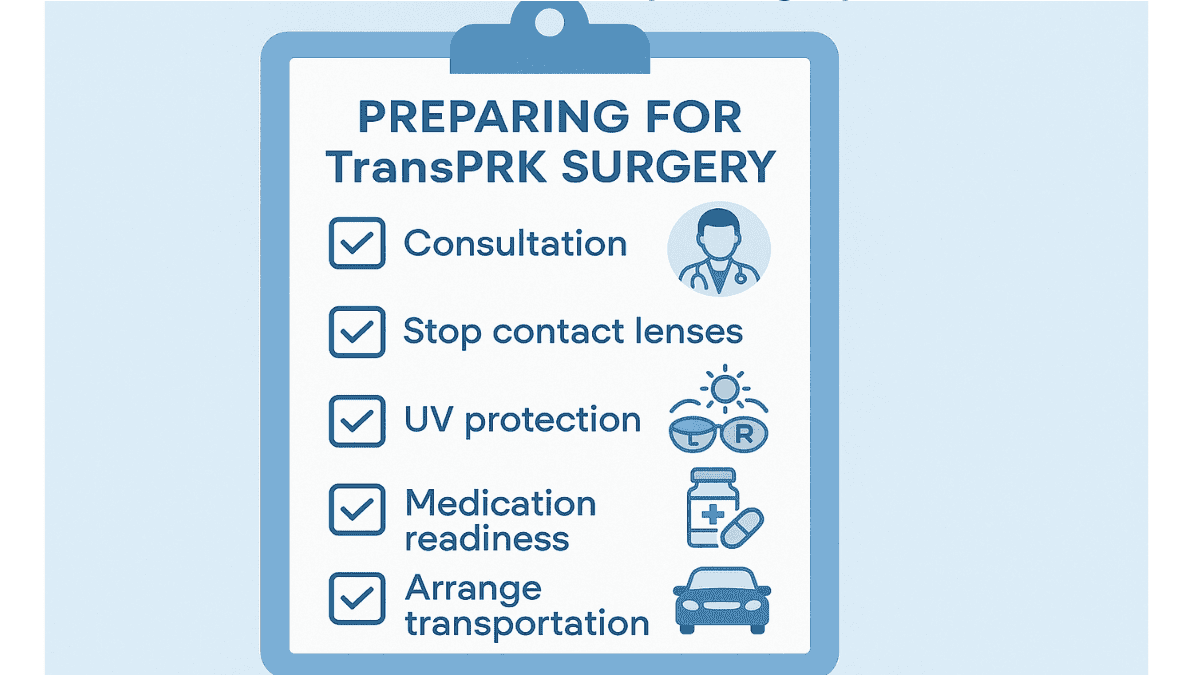
Choosing TransPRK eye surgery is a significant decision. Thorough preparation contributes to a smoother experience and helps achieve optimal long term visual outcomes. Consider these key aspects as you get ready for your laser refractive surgery.
Finding a qualified surgeon and reputable clinic is paramount. Seek a specialist in refractive surgery with proven experience in TransPRK, possibly using systems like the Schwind Amaris laser. Inquire about their expertise, the technology they employ, such as the specific Amaris laser model, and their patient outcomes.
Many centers offer an initial eye consultation, often complimentary, providing a chance to meet the team. This is also where you might learn if the clinic’s philosophy aligns with a “veni vidi” approach—aiming for patients to clearly see and conquer their vision challenges. Such a consultation is invaluable for assessing compatibility and comfort.
The pre-operative eye consultation itself is critical for this step procedure. Your surgeon will conduct extensive tests to confirm your suitability for TransPRK surgery. This is also your main chance to ask questions; prepare a list to cover all your concerns about this advanced surface technique.
Inquire about the expected visual results for your prescription, recovery details, specific risks, and included follow-up care. Managing expectations is also crucial. While TransPRK boasts high success rates for those seeking to improve vision, perfect 20/20 vision, though common, is not guaranteed for every individual, especially those with a kornea yüzeyi normalden (cornea surface that is abnormal) or with very yüksek numaralara (high prescriptions).
Discuss realistic goals with your surgeon and prepare for the recovery. Understanding potential discomfort and vision fluctuations aids in a calmer recovery. Lastly, consider the cost, as laser eye surgery is an investment in your vision and quality of life.
Clarify what the TransPRK price includes: pre-operative exams, the transepithelial photorefractive keratectomy itself, medications, and all follow-up visits. Explore financing options if necessary. Clarity on these elements builds confidence as you proceed with this important step to correct refractive issues.
Conclusion
TransPRK surgery represents a significant step forward in laser vision correction technology. It provides an advanced ‘no-touch’, single step procedure to improve vision without creating a corneal flap. This flapless approach is a considerable advantage for individuals with thinner corneas (ince olan), active lifestyles, or those wishing to avoid flap-related issues.
While TransPRK recovery may require more patience than LASIK, the long term benefits are compelling. Enhanced corneal stability and the high quality of vision achievable make transepithelial photorefractive keratectomy an excellent option for many. People seeking freedom from glasses and contact lenses, including those whose kornea yüzeyi normalden daha dik (cornea surface is steeper than normal), might find TransPRK highly suitable.
Ultimately, if you are considering laser refractive surgery, a detailed eye consultation with an experienced surgeon is essential. This discussion will help determine if TransPRK, often performed with systems like the Schwind Amaris laser, is the most appropriate path to achieve your vision goals. The aim is a future with clearer sight, making everyday moments easier to appreciate.
FAQ
TransPRK is a flapless, no-touch laser vision correction technique that uses an excimer laser to reshape the cornea. Unlike LASIK, it doesn’t involve creating a corneal flap, reducing flap-related risks.
The procedure itself is painless due to numbing eye drops. Some discomfort, light sensitivity, or tearing may occur for 2–3 days after surgery as the epithelium heals.
The laser treatment takes less than one minute per eye. The full procedure, including preparation, typically lasts about 15–20 minutes.
Initial healing occurs in 3–5 days, but full visual stabilization can take several weeks. Most patients experience significant improvement within the first month.
Candidates include individuals with stable vision, thin corneas, active lifestyles, or those not suitable for LASIK due to flap risks or dry eye concerns.
Yes. TransPRK preserves more corneal tissue by avoiding a flap, making it especially suitable for patients with thinner-than-average corneas.
Yes. TransPRK can effectively correct myopia, hyperopia, and astigmatism. Its suitability for high prescriptions depends on corneal thickness and shape.
The all-laser approach eliminates manual scraping or alcohol application, resulting in a smoother corneal surface and potentially faster epithelial healing.
Many patients achieve 20/20 or near-perfect vision without correction. However, results vary based on pre-op prescription and individual healing response.
Temporary side effects may include dry eyes, light sensitivity, blurry vision, and glare. These typically improve as the eye heals.
No. The bandage contact lens and prescribed antibiotic drops help prevent infection. Not having a flap may even reduce long-term complication risks.
Most patients can resume light activities after 5–7 days. Tasks requiring sharp vision may need to wait until visual clarity improves further.
Yes. Follow-up visits ensure the cornea is healing properly and allow your surgeon to monitor vision improvement and address any concerns.
Studies suggest TransPRK may cause fewer or less severe dry eye symptoms compared to LASIK, especially due to the absence of a corneal flap.
Yes. If minor refractive errors persist or vision changes over time, enhancement procedures may be considered after full healing.